Keywords
Virtual reality; Physiotherapy; Stroke; Upper limb
Introduction
The stroke is one of the most common diseases of the central nervous system and a major cause of disability. Current demographic projections point to the fact that in the future there will be seen a gradual increase in the number of episodes of stroke among Polish population. Expected higher number of such cases is a challenge for physiotherapy, and therefore calls for introduction of innovative methods for rehabilitation of patients after stroke. With the development of science and technology neurological patients are faced with new possibilities of regaining psychomotor fitness. It is obvious that any additional form of improving patient's motor functions is no substitute for individual work with a physiotherapist, which is adapted to the individual patient's needs. However, there is a clear need to search for new attractive and modern forms of medical rehabilitation, should they only supplement modified forms of traditional neurological physiotherapy. Over 69% of cerebrovascular incidents result in limitations of motor functions in the upper extremity on the side opposite to the cerebral hemisphere where the incident occurred. Paresis of the upper limb significantly reduces quality of life, on top of that it greatly impedes or prevents performing the activities of daily living (ADL) [1]. One of the main tasks in rehabilitation of patients after stroke is to maximize the restoration of functional efficiency of the paretic upper limb.
Physiotherapy in virtual reality
The passage of time and technological progress made computer technology become ever-present in the lives of majority of people. This form of progress has also been used in medical rehabilitation as physiotherapy in virtual reality. Virtual reality (VR) is a computer-generated, interactive simulation that maps the real environment by affecting human senses, and shows all activity in real time and with real speed. VR sends the user a great number of sensory information comparable to authentic experiences [2]. This modern computer technology emulates learning process in the real world, while allowing the addition of extrinsic feedback and increasing the frequency, duration, and even intensity of an exercise [3]. Virtual environment (VE) enables the user to have the opportunity to interact with objects and situations produced by the hardware. A distinctive platform creates well-defined and customized activities, combining factors such as intensity, variation and specificity of the tasks described as significant for increasing plasticity of the brain. For about 15 years physiotherapy of neurological patients in virtual environment has been used with good results [2,4,5]. VR technologies allow creation of a simulated environment so that proper adjustment of exercise intensity and feedback would provide the patient with safe and effective training and rehabilitation [6]. Using virtual reality can proceed with "immersion" or without "immersion". Both forms allow for different ways to participate in virtual physiotherapy. "Immersion" in the three-dimensional environment is defined as placement of the user in such environment via a device called head mounted display (HMD), which can significantly increase the "sense of presence" in the VR, which in turn, brings about the impression that performed exercises seem very real. In virtual training without the "immersion" the exercises take place in a two-dimensional environment by using a standard computer screen or wall screen. The main advantage of this form of therapy is low cost of specialized software and the chance for patients to self-exercise [7,8].
Aim
The main goal of the above article is to attempt to preliminarily analyze the impact of physiotherapy in virtual reality on improvement in motor performance of the paretic upper limb in patients after ischemic stroke. An additional aim of this work is to determine the effect of exercises in a virtual environment on nonparesis upper limb in the same group of patients.
Research Method
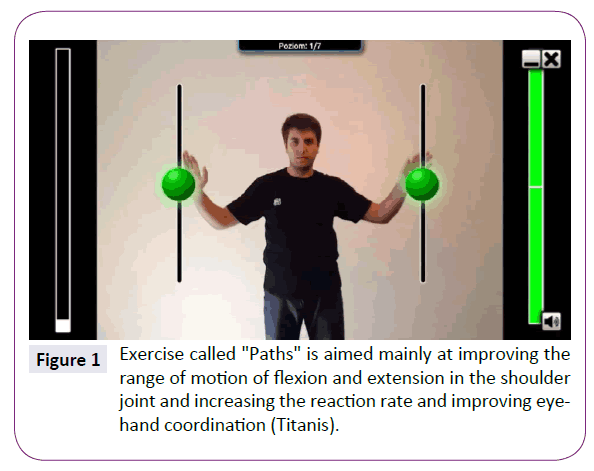
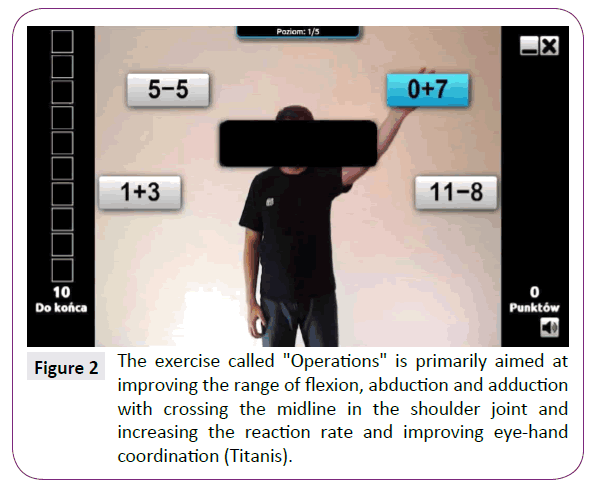
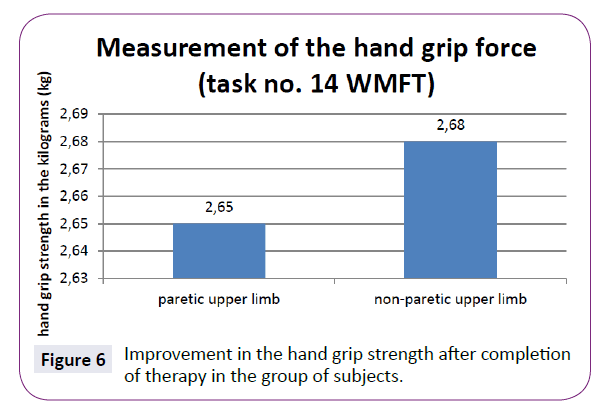
During the study there was used a computer program "Neuroforma" from Titanis Ltd. which enables physiotherapy in virtual environment. The program uses Motion Capture technology, which allows you, by means of a camera, to track and analyze the movement of objects that are within range and Augmented Reality system that connects the real world with computer-generated environment. "Neuroforma" is an innovative program that aids the process of physical-cognitive rehabilitation in virtual reality and dynamic feedback. Exercises with "Neuroforma" take place in virtual environment without "immersion", and the program itself is dedicated to work with neurological patients, among others, after a stroke. During therapy the patient is sitting in front of a wall screen, where he can watch his own mirror reflection while there is a multitude of virtual objects moving around him. The user's job is to catch, evade, hit or track those visualizations. Thanks to modern technology, the program provides instant feedback that indicates whether the exercise was done correctly. "Neuroforma" system was designed as a set of medical mini-games that are intended to improve motor functions of the upper limbs while engaging cognitive functions e.g. the processes of perception, planning, attention and memory. At the same time, the system also performs the dual task paradigm: cognitive and motor rehabilitation, and allows and enables the physiotherapist to oversee the work of the patient and correct the patient's mistakes. The program reminds motion games where the main task is to control the upper limbs instantaneously, so as to score the highest possible number of points. For example, motion games of Neuroforma program, as presented in Figures 1-3. The difference between "Neuroforma" and other games of this kind is that the user's activity is not random, but designed and adapted to his needs. It should be noted that both the patient and therapist have the possibility to control and track the results of therapy. When using the program indicators such as exercise time speed of response, efficiency of movement and the amount of errors are recorded and stored. It is not insignificant that the system is motivating for the patient and allows you to combine pleasant way of spending time and effective physical exercise. A characteristic feature of "Neuroforma" are two forms of the system: home version of the program and telerehabilitation module used in the centres and rehabilitation wards. Neuroforma software has been licensed for use at the rehabilitation ward in the Department of Social and Medical Rehabilitation and Treatment in 42 Mogilenska Street in Poznan.
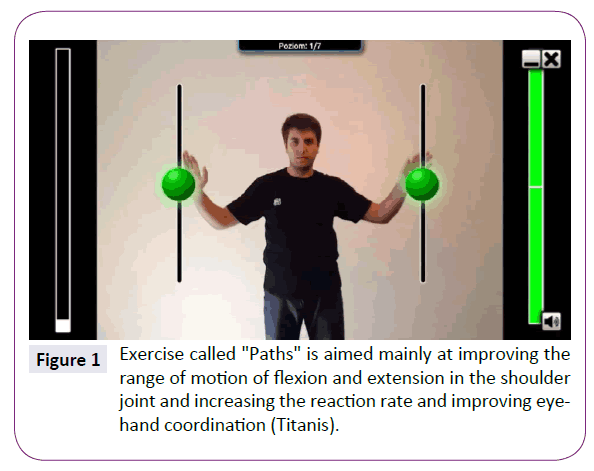
Figure 1: Exercise called "Paths" is aimed mainly at improving the range of motion of flexion and extension in the shoulder joint and increasing the reaction rate and improving eyehand coordination (Titanis).
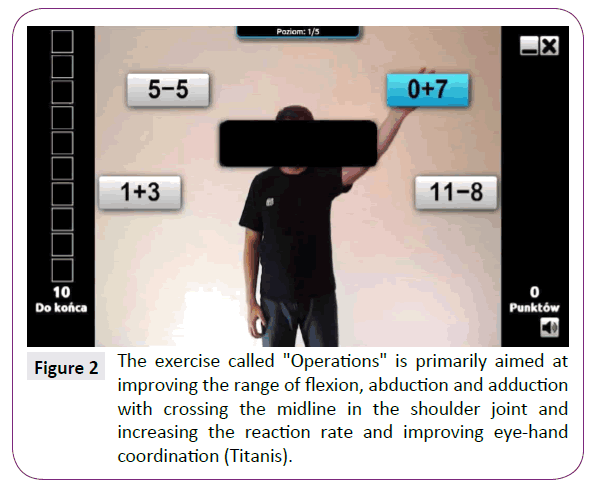
Figure 2: The exercise called "Operations" is primarily aimed at improving the range of flexion, abduction and adduction with crossing the midline in the shoulder joint and increasing the reaction rate and improving eye-hand coordination (Titanis).

Figure 3: The exercise called "Boxing" is mainly aimed at improving the range of motion in flexion.
In order to evaluate the effect of physiotherapy in virtual reality on the upper limb motor performance in patients after ischemic stroke Wolf Motor Function Test (WMFT) was used. For each patient the above measuring instrument is used twice: for the first five days and in the last three days of hospitalization in the rehabilitation ward. WMFT is a quantitative scale, consisting of 17 timed tasks and functional exercises. The total time of completing the test is approx. 30 minutes [9]. WMFT tasks are divided into 16 exercises "against time" and one of the tasks aimed to assess the strength of the squeeze of the hand. Tasks "against time" were assessed using a stopwatch, and strength measurement was made using an electronic dynamometer Charder MG4800.
Patient examinations using the Ashworth Scale for Grading Spasticity were done twice: during the first five days and during the last three days of hospitalization in the rehabilitation ward.
During the study, the non-paretic upper limb was treated as a basis for comparison in relation to the paretic upper limb, which was the main subject of research in this project.
Group of study participants
The study included 13 patients after ischemic stroke, who remained in the rehabilitation ward in the Department of Social and Medical Rehabilitation and Treatment in 42 Mogilenska Street in Poznan. Patients were admitted to rehabilitation ward because of, among others, limited motor functions of the paretic upper limb. Inclusion criteria for participation in the study were as follows: post ischemic stroke state, paresis of the upper extremity and age between 50 and 85 years. The exclusion criteria include: significant spasticity of the paretic upper limb according to Ashwort scale (degree 3 and 4), over 10 years that elapsed after stroke, and significant cognitive impairment which hinders communication. The whole group participated in the same form of conventional physiotherapy during the stay in the rehabilitation ward. Characteristics of the study participants are presented in Table 1. While staying at the rehabilitation centre the patients from the study group underwent a six-week rehabilitation program, containing kinesiotherapy, physical therapy, therapeutic massage and 10 hours of physiotherapy in virtual reality divided into therapy sessions. In the course of rehabilitation sessions with the program "Neuroforma" in majority of the exercises the patients used both the upper limb with paresis and the limb without paresis. Only two out of eight motion games used in the project were focused exclusively on improving the affected upper limb. The research is still carried out in this facility.
| Characteristics |
Group of study participants |
| Average age (in years) |
68 |
| Average time that elapsed from stroke (in years) |
3 |
| Time since stroke |
| 1-5 years |
10 |
| 5-7 years |
3 |
| Paresis on the right /left side |
7/6 |
| Gender |
| Men/Women |
9/4 |
| Upper limb dominant before Stroke |
| right/left |
12/1 |
Table 1: Characteristics of the study participants.
Results
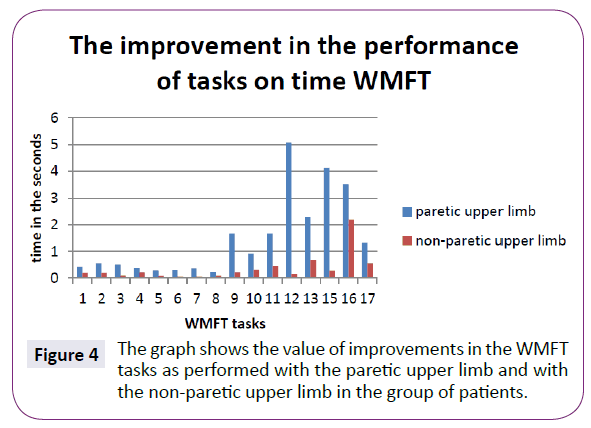
As shown in Figure 4 participants from the study group performed faster all WMFT tasks (with the paretic upper limb as well as with the non-paretic upper limb ), which assessed the rate of completing a given task in seconds, as compared to the score recorded at the beginning of the rehabilitation treatment. Greater improvement was noted in activities performed with the paretic upper limb.
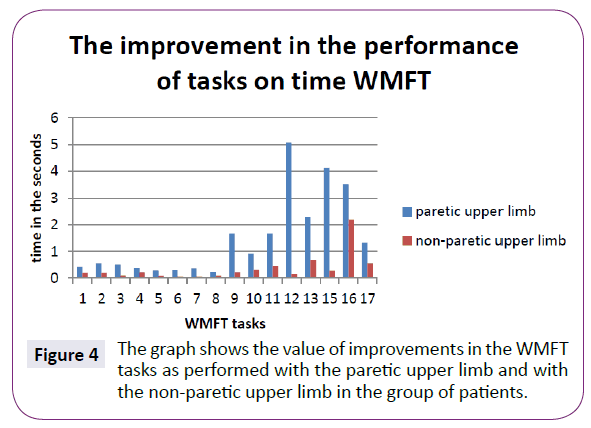
Figure 4: The graph shows the value of improvements in the WMFT tasks as performed with the paretic upper limb and with the non-paretic upper limb in the group of patients.
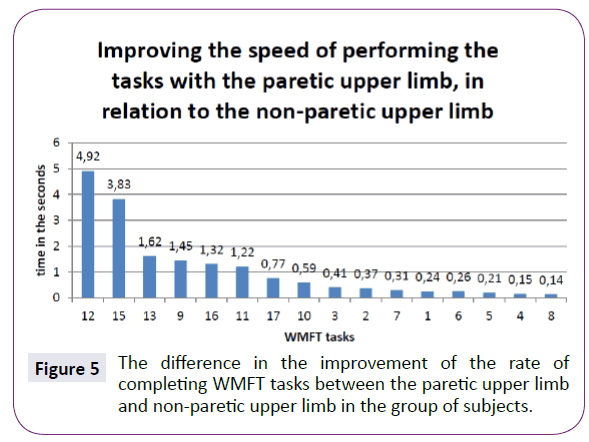
As presented in Figure 5 examined people performed faster all WMFT tasks with the paretic upper limb when compared to the non-paretic upper limb which assessed the rate of completing a given task in seconds, as compared to the score at the beginning of rehabilitation treatment .That difference can be seen most clearly in tasks: number 12 (placing two checkers on third checker), number 15 (turning the key in the padlock to the left and right with a pincer grip) and number 13 (reversing three cards with a pincer grip). The Table 2 shows the difference in executing Wolf
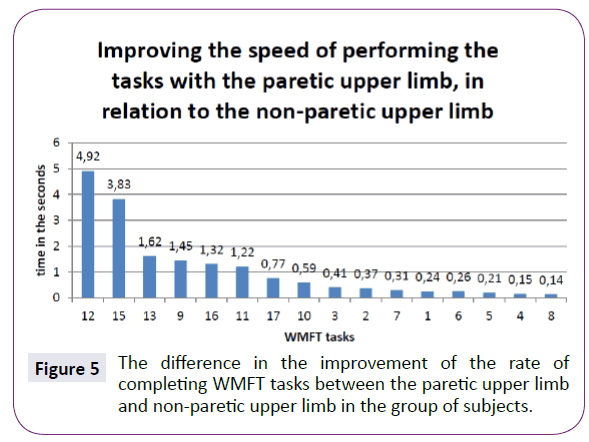
Figure 5: The difference in the improvement of the rate of completing WMFT tasks between the paretic upper limb and non-paretic upper limb in the group of subjects.
| WMFT Task the values given in seconds (s)or kilograms (kg) |
Paretic upper limb |
Non-paretic upper limb |
| 1 |
+ 0,43 |
+0,19 |
| Forearm to table (side) |
| s |
| 2 |
+0,56 |
+0,19 |
| Forearm to box (side) |
| s |
| 3 |
+0,51 |
+0,1 |
| Extend elbow (side) |
| s |
| 4 |
+0,37 |
+0,22 |
| Extend elbow (weight) |
| s |
| 5 |
+0,29 |
+0,08 |
| Hand to table (front) |
| s |
| 6 |
+0,31 |
+0,05 |
| Hand to box (front) |
| s |
| 7 |
+0,36 |
+0,05 |
| Weight to the box |
| s |
| 8 |
+0,23 |
+0,09 |
| Reach and retrieve (front) |
| s |
| 9 |
+1,67 |
+0,22 |
| Lift can (front) |
| s |
| 10 |
+0,91 |
+0,32 |
| Lift pencil (front) |
| s |
| 11 |
+1,67 |
+0,45 |
| Pick up paper clip(front) |
| s |
| 12 |
+5,07 |
+0,15 |
| Stack checkers (front) |
| s |
| 13 |
+2,29 |
+0,67 |
| Flip cards (front) |
| s |
| 14 |
+2,65 |
+2,68 |
| Grip strength |
| kg |
| 15 |
+4,11s |
+0,28s |
| Turning the key in lock (front) |
| s |
| 16 |
+3,52s |
+2,2 s |
| Fold towel (front) |
| s |
| 17 |
+1,33 s |
+0,56 s |
| Lift basket (standing) |
| s |
Table 2: The difference in executing Wolf Motor Function Test before and after physiotherapy in all examined people (peaks on the graph are expressed in seconds or kilograms).
Motor Function Test tasks by paretic and non-paretic before and after physiotherapy in examined people.
From Figure 6 we can see that in the group of subjects it was observed that the output value of the gripping strength of the paretic hand has increased by 2,65 kg, and of the non-paretic hand by 2,68 kg as compared to the score recorded after completing the rehabilitation program. As a result, it was found that exercises in virtual reality in a similar way have improved gripping force of both the paretic hand and the hand not affected by paresis.
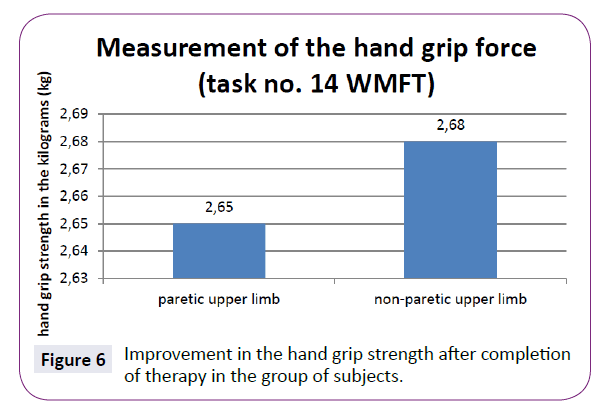
Figure 6: Improvement in the hand grip strength after completion of therapy in the group of subjects.
Paretic upper extremity of each of the study participants was examined using Asworth scale. Among the subjects of the study was found "0" - no increased tone; '1' - increased muscle tone causes a 'catch' when the limb is moved in flexion or extension;'2' – the tone is more pronounced but the limb can be moved easily. After completion of virtual therapy there were observed no changes in the subjects' muscle tones.
Discussion
Research on the effects of virtual rehabilitation on improvement in the efficiency of upper limb after stroke have demonstrated positive effect of physiotherapy in virtual environment on motor re-education and improving upper limb function.
The study described above was conducted to initially analyze the impact of physiotherapy in virtual reality with Neuroforma software, on the efficiency of the paretic upper limb after stroke.
Due to small number of the study participants and a parallel, conventional rehabilitation unfortunately we cannot determine to what extent the training in virtual environment had impacted the improvement in performance of the WMFT tasks. The research helped to check the suitability of the program for future use in rehabilitation wards and in the patient's home. Although no scientific reports on self- use of Neuroforma at home were found, in our opinion it is an useful and safe, after appropriate instructions, tool to support home-rehabilitation. Furthermore, the survey helped to analyze the functioning of the Neuroforma program in practice and the reaction of participants to this kind of rehabilitation therapy. It was observed that none of these people felt any side effects associated with the use of Neuroforma. The program was well received by the participants. After the end of treatment were not observed in participants neither increase nor reduction in the paretic upper limb spasticity, or the appearance of pathological compensation. The program enables the design of therapeutic trainings tailored to each patient's functional status. It should be noted that both the patient and therapist have the ability to control and follow the results of therapy. While using the program the saved data includes parameters such as: exercise duration, response rate, efficiency of movement and the number of errors. What is significant is the fact that the system is motivating for the patient and allows you to combine a pleasant way of spending time and an effective way of exercising. In the future, we plan to conduct a study on the use of Neuroforma in improving paretic upper limb after stroke involving a larger number of patients.
Laver and al. conducted a review of studies carried out in the years 2004-2014, which were aimed at comparing the effects of physiotherapy in virtual environment with conventional forms of rehabilitation or lack of rehabilitation. The compilation covered 37 research projects and 1,019 participants after stroke. The research was designed to assess the impact of this type of therapy on improving the efficiency of upper limb, gait function, cognitive functions and activities of daily life. In the course of preparing the research paper there have been used, among others, the following databases: MEDLINE, EMBASE, AMED and CINAHL. The most common type of intervention used in the study was upper limb therapy. According to the authors twelve studies have proven that therapy in virtual environment, which aimed to improve the efficiency of the upper limb, brought about better effects than traditional forms of therapeutic rehabilitation (SMD - standardized mean difference 0.28; 95% CI - confidence intervals 0.08 to 0.49). On the other hand, 9 trials demonstrated that treatment with virtual reality, focused on improving upper limb functionality, brought about significant effects if compared to lack of rehabilitation (SMD 0.44, 95% CI 0.15 to 0.73). The authors, however, point out that despite having conducted many research projects, the evidence is still insufficient to definitely conclude that physiotherapy in virtual reality is an effective form of rehabilitation for patients after stroke. The authors have identified the low quality of evidence on the positive impact of virtual rehabilitation on improving motor functions of the paretic upper limb after stroke. The low quality of evidence have been caused by: a small number of participants in the research projects, inconsistent results across studies and unsatisfactory descriptions of study details [10].
Desrosiers and al. compared the sensorimotor skills of the non-paretic upper limb in elderly stroke patients with healthy, elderly people (compatibility in terms of gender and age). The project was attended by 43 people after stroke, and 43 people were qualified for the comparison group. Patients from the study group meet conditions such as paralysis or hemiplegia, age over 60 years, right-handedness, episode of stroke from 0.5 to 4 years earlier. Subsequent to testing the patients after stroke there were discovered significant deficits in the following parameters: gross manual dexterity, fine manual dexterity, motor coordination, global performance and thumb kinesthesia (P<0.01 is P<0.0001). There were, however, no clinically or statistically significant differences in terms of: grip strength (P<0.81), static and moving two-point discrimination (P=0.21 and P=0.12) or touch / pressure threshold (P<0.91). Many factors (frequency of use of the unaffected hand, sensorimotor interaction tasks, severity of the deficits in corticifugal projections, and deficits in postural stabilization) could interact with one another and ultimately affect the test results. The authors emphasize that during the therapy of patients after stroke attention should be paid to improving the sensorimotor functions of the non-affected upper limb, but it cannot be done at the expense of re-education of the paretic upper limb [11].
Conclusions
The study was aimed to initially describe the impact of physiotherapy in virtual reality on upper limbs motor skills in patients after ischemic stroke. Data analysis allowed to draw the following conclusions:
1. Virtual reality therapy can be used as a good method complementary to physiotherapy treatment applied in patients after ischemic stroke.
2. For a more detailed assessment of the effectiveness of the method of physiotherapy in virtual reality, it is advisable to conduct studies involving larger numbers of patients.
7359
References
- Kiper P, Baba A, Agostini M, Turolla A (2015) Proprioceptive Based Training for stroke recovery. Proposal of new treatment modality for rehabilitation of upper limb in neurological diseases. Archives of Physiotherapy 5:6.
- Viau A, Feldman AG, McFadyen BJ, Levin MF (2004) Reaching in reality and virtual reality: a comparison of movement kinematics in healthy subjects and in adults with hemiparesis.J NeuroengRehabil14: 11.
- Sisto SA, Forrest GF, Glendinning D (2002) Virtual reality applications for motor rehabilitation after stroke. Top StrokeRehabil 8: 11-23.
- Shin JH, Ryu H, Jang SH (2014) A task – specific interactive game – based virtual reality rehabilitation system for patients with stroke: a usability test and two clinical experiments. Journal of NeuroEngineering and Rehabilitation 11: 32.
- Subramanian SK, Levin MF (2011) Viewing medium affects arm motor performance in 3D virtual environments. J NeuroengRehabil 8: 36,44.
- Crosbie JH, Lennon S, McGoldrick MC, McNeill MDJ, McDonough SM (2012) Virtual reality in the rehabilitation of the arm after hemiplegic stroke: a randomized controlled pilot study. ClinicalRehabilitation 26: 798,806.
- Smith CM, Read JE, Bennie C, Hale LA, Milosavljevic S (2012) Can non-immersive virtual reality improve physical outcomes of rehabilitation? PhysicalTherapyReview 17: 1.
- Crosbie JH, Lennon S, McNeill MDJ (2004) Virtual reality in the rehabilitation of the upper limb after stroke: the user’s perspective. Oxford215,224.
- Opara J (2010) Clinimetrics in strokes. Academy of Physical Education in Katowice Publishing,Klinimetria w udarach mózgu. Wydawnictwo Akademii Wychowania Fizycznego w Katowicach 83: 118.
- Laver K, George S, Thomas S, Deutsch JE, Crotty M (2015) Virtual reality for stroke rehabilitation: an abridged version of a Cochrane Review. Eur J PhysRehabil Med.
- Desrosiers J, Bourbonnais D, Bravo G, Roy PM, Guay M (1996) Performance of the 'unaffected' upper extremity of elderly stroke patients. Stroke 27: 1564,1570.