Keywords
Wound; Wound infection; Wound dressings; Hydrogel dressings; Antimicrobial dressings
Introduction
A wound or trauma happens once skin, the largest human organ, is broken at any accident or surgery. Generally, wounds, especially serious wounds needs to be taken care for recovery and in case of germ infection [1,2]. It is necessary to treat and monitor the wounds if they are bleeding, large, deep or infectious [3]. The recovery and management of severe wounds is a complicated and collaborative process including infectious prevention, germ treatment and treatment strategy [2,4], with the involvement of doctors, nurses, patients, pathologists and wound specialists. Particularly, the application of wound dressings play very critical roles in wound healing and infectious prevention [5]. There are many different types of wound dressings such as silver-containing hydrophilic fiber dressing, antibacterial dressing and wet dressing. Based on different materials, they can be classified as foams [6,7] gauze [8], transparent films [9,10], alginates [11], composites [11], hydrocolloids [12,13] and hydrogel [5,12,14-17]. These dressings display their own advantages and disadvantages in wound treatment. They are used so frequently in our routine wound treatments. However, it is a tough challenge for doctors and nurses to routinely choose a good and right wound dressing for the right wound situation at the right time. Meanwhile, a good dressing with high quality and ideal function will speed up wound healing, reduce patients’ pains and prevent wound from germ infection [17,18]. Here, we discussed different types of wounds, various wound dressings and their applications in wound treatment and recovery.
Different types of wounds
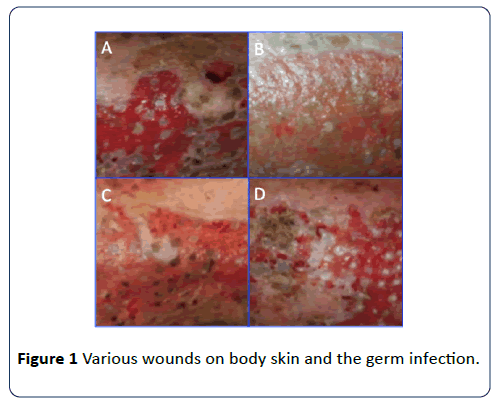
Skin is our organ that directly prevents and protects us from germ invasion and infection. The skin broken in an accident could result in wound happening. Up to different accidents, cases and situations, wounds can also be classified as different types from mild, moderate to severe wounds, from small to large wounds, from shallow to deep wounds, from noninfectious to infectious wounds, from burns, contusion, knife injury, crushing injury, needling injury, to gunshot wounds, from acute to chronic wounds (Figure 1) [3,19]. For example, acute wounds such as slight abrasion, knife wound, slight scald, skin breaking, and the initial stage of the wound after operation, suddenly happen and quickly heal. Chronic wounds such as ulcerative wounds, diabetic foot ulcer, venous lower extremity ulcer, arterial lower extremity ulcer, chronic radiation injury and deep burn or scald [7,20,21], are the wounds with the healing process lasting much longer time [2]. No matter what type of wounds or traumas and in case of germ invasion through skin, the wounds need to be cleaned and debrided to remove dirt and contaminates. Sterilizing and covering wound is important to prevent infection and inflammation [20,22]. Certain infectious wounds such as gunshot usually need special wound treatment and management to prevent germ infection.
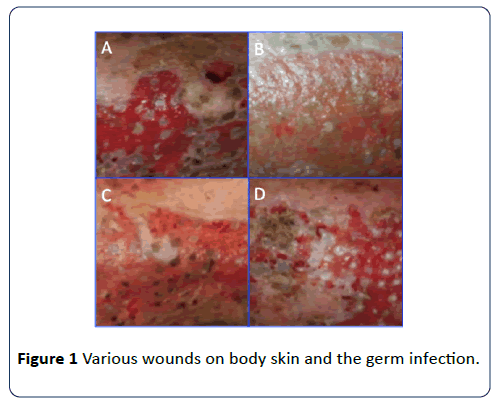
Figure 1: Various wounds on body skin and the germ infection.
Wound healing
Wound healing is a complicated process, with different strategies in treating different types of wounds. According to trauma area, infectious situation and medical treatment, wound healing can be divided into different categories including primary healing, secondary healing and subeschar healing [1,2]. Primary healing occurs when there are less tissue defects in wounds, neat wound margins with no infection, sutured wound with strict wound surface involution [1,3]. Surgical incision healing is a typical example of primary healing. Secondary healing often occurs when there is large wound area in wounds, large tissue defects, and irregular wound margin with hard wound surface involution or germ infection. These wounds are healed via filling tissue defects with granulation tissues. This type of wound healing is also known as indirect wound healing. Inflammation is obviously observed in secondary healing due to persistent germ infection and degenerative tissue necrosis [23,24]. Normally, tissue regenerates after germ infection is controlled and necrotic tissue is removed. There are large wound area, obvious contraction, longer healing time and more scar tissue in secondary healing. The blood, exudate or necrotic tissue on the wound surface becomes dried and forms scab. In the absence of infection, wound healing can act as subeschar healing [20]. The regenerated epidermis grows under scab from the edges of wound and covers original dermal connective tissues at wound surface area or newborn connective tissues filling in dermal defect. The scab falls off when the reepithelialization is completed. Eschar is usually dry. The dry eschar can prevent germs from growth, have certain protective effect on wounds and promote wound healing. However, scab may obstruct local drainage and further hinder wound healing if there is more subeschar exudate or germ infection [7,19].
Applications of wound dressings
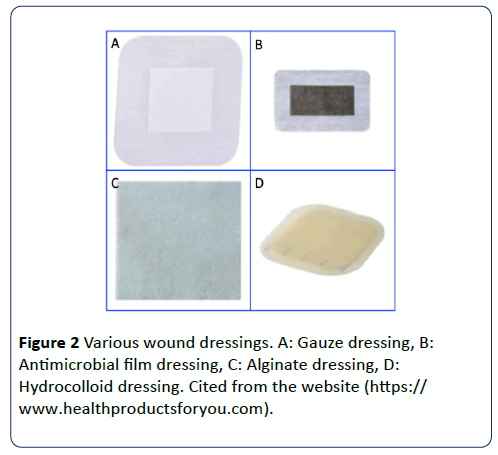
Wound recovery and management is always a challenge to wound patients, specialists and doctors. In our routine work, we always have to face different patients with different types of wounds. Mostly, wound healing is always accompanied by wound infection [4]. Wound dressings play critical roles in wound treatments. A good dressing can promote wound healing and prevent germ infection [10,23,25,26]. Moreover, we often need to switch different types of wound dressings during whole process of a case treatment, or a dressing need to be used together with other dressings to create a good environment for wound recovery and wound protection. There are many different wound dressings available on market (Figure 2 and Table 1). How to choose a right type of wound dressing is very difficult and skilled. A wound specialist with rich experience understands most of the types of wound dressings with their rationale, applicability, efficacy and indications. He can decide to choose the right type one for wound treatment by assessing the wound situation of each patient. In the process of wound treatment, there are many different types of dressings such as foams [15], gauze [8,14], transparent films [9,17], alginates [17], composites, hydrocolloids [27] and hydrogel (Table 1) [7,16]. Whether to use a particular dressing is the most difficult in wound management. Thus, it is important and necessary to understand the types and characteristics of dressings and their indications, and the advantages and disadvantages of each wound dressing. Here, we will introduce various wound dressings commonly used in our case treatments.
Table 1: The general types of wound dressings.
| Types |
Characteristics |
Indications |
Advantages |
Disadvantages |
| Foams |
Multilayer structure
Good absorption property, with a moist and warm environment for wounds. |
Partial or full-thickness injury. Medium to massive exudation of wounds. Absorbing effluent. |
No wound adherence.
Low replacement frequency.
Absorbing large amount of exudates to reduce the influence of exudates and impregnation on wounds.
Comfortable and easy to use.
Good compliance, easy to tear off without hurting the skin. Insulation and heat preservation buffer external impulse/pressure.
Prolong the use time of wound dressing. |
Exudation may cause skin immersion around the wound.
Not suitable for eschar and dry wounds
Need external dressing to fix the non-adhesive edge.
Opaque, with no observation of the wound directly.
High possibility of bacterial invasion.
Dressing removal may damage the new tissue and causes pain. |
| Gauze |
Woven/non-woven materials, mostly cotton.
Used to treat wound exudate, wound wrapping and protection. |
Suitable for one-time use in cleaning, hemostasis bandaging or hygienic care of surgical or local wounds in medical units.
One-time use for operation and wound care in medical units. |
Affordable and easily available.
Able to protect wounds and reduce bacterial invasion.
Simple to use and suitable for many kinds of wounds.
Widely used in clinic.
Cheap and suitable for various consumption levels. |
Frequent replacement and wound bed adherence.
Not for wet wound healing.
High possibility of bacterial invasion.
The granulation tissue of wound is easy to grow into the mesh eye of gauze.
Dressing removal may damage the new tissue and cause pain.
No obvious promoting effect on wound healing.
Often need to be combined with other types of dressings. |
| Transparent membrane |
Polymeric materials Translucent, allowing oxygen and water vapor passing through,preventing water and germ from passing through. |
Suitable for treating superficial wounds. Protection of skin prone to abrasion or external contamination.
Maintenance of the first layer dressing. |
Good adherence. Prevent the friction and bacterial infection of wound bed.
Transparency and easy wound observation with no removal.
Keeps humidity in the wound bed surrounding skin.
Cheap price, good fit.
Conducive to self-dissolving debridement.
Prevent the wound bed friction and bacterial contamination. |
Wound seal resulting in peripheral skin immersion and impregnation of surrounding skin.
Wound bed adherence.
Not suitable for severe exudative wounds.
Not for severe exudative wounds. |
| Alginates |
Alginate is extracted from algae. Woven or nonwoven materials
strip and sheet dressings. |
Wounds with partial to full-thickness injuries.
Medium to large exudates.
Pit/hole or sinus tract. |
Strong exudate absorption capacity, used for infectious wound, with no wound adherence.
Promoting autolysis debridement.
Providing a wet healing environment to keep nerve endings moist.
Relieve pain, avoid dehydration and promote epithelial regeneration.
Form hydrate with necrotic tissue to help wound autolysis and debridement.
Easy to use and remove, no toxicity, no allergy. |
Need two layers of dressings causing wound bed dry or dehydration.
Misuse may cause tissue necrosis.
Not for small amounts of exudation or dry eschar. Need a second dressing.
Not easy to remove the residual dressing.
High cost. |
| Composites |
A combination of any kind of dressings. |
Grade II burn and small area Grade III burn wounds, surgical wounds, infectious wounds, refractory chronic wounds for debridement of rotten granulation wounds and old granulation wounds. |
Easily use and available.
Used as one or two layers of dressing.
Used for a variety of wound types.
Good permeability and compliance.
Strong absorptive capacity.
Continuous debridement, accelerating necrotic tissue exfoliation.
Control infection and promote wound healing.
Effective protection of skin grafts to prevent infection and necrosis. |
High cost.
Low cost performance.
Low flexibility of indication.
Frequent replacement once a day.
Not suitable for wounds with vascular exposure on the surface, especially those with partial vascular embolism and necrosis. |
| Hydrocolloids |
Colloidal particles. Certain exudative absorption capacity, strong stickiness. |
Superficial, moderately deep wounds with small to moderate exudation and desquamated or necrotic tissue. |
Provide a moist environment for clean wounds and granulation tissue.
Promote autolysis debridement of necrotic tissue.
Providing hypoxic and wet healing environment
Flake self-adhesive, sealing wound bed, without the second layer of dressing, to prevent bacterial invasion and waterproof.
Comfort and reduce friction, relieve pain, and promote epithelial migration and granulation tissue growth.
Good compliance and easy to use. |
The strong stickiness resulting in skin injury.
Not for mass exudation and infecting wounds.
Opaque, not easy to observe the wound.
Not suitable for infectious wounds and wounds with exposed tendons and bones.
Dressing removal will affect the fragile skin around.
Not suitable for wounds with more exudation and easy to impregnate the skin. |
| Hydrogel |
Hydrogel sheet or amorphous with rich water used for auxiliary and autolysis debridement and softening eschar. |
Partial or full-thickness injury.
Necrotic or desquamate wounds small to medium exudation.
Hydration promotes self-dissolving debridement. |
Positively providing water to dry wounds and keeping wound moist. No wound adherence.
Promoting autolysis debridement for scab debridement.
Conducive to epithelial migration and granulation growth Non-sticking wound.
Pain relief pretecting germ infection. |
Poor absorptive capacity of exudates.
Not for severe exudative wounds and infectious wounds.
No bacterial barrier.
Easy to cause skin immersion around.
A second layer of dressing is needed.
The dressing color will turn green, which is easily confused with Pseudomonas aeruginosa infection. |
Foam dressings
Foam dressings are made of polymer material and are usually multi-layer structures, which are consisting of anti-adhesion wound contact layer, infiltration layer and waterproof and germresistant layer (Table 1) [6,15,24]. The surface is often covered with one layer polymeric semi-permeable membrane. Some of them are self-adhesive, with the main ingredients being silica gel and so on. Its action mechanism is that the absorptive foam absorbs a large amount of exudate, reduces infiltration, and provides a moist, warm and closed wound healing environment. Foam dressing is suitable for wounds with medium to large amount of exudates. The dressings can be used for the treatment and prevention of pressure ulcer, diabetic foot ulcer, skin donor area, mild burn, skin transplant, venous ulcer etc. The advantages of foam dressing are able to provide a moist and closed healing environment and support autolysis debridement. And also with its high absorptivity, it can absorb medium to large amount of exudates and reduce the influence of exudates and impregnation on wounds. A low frequency of dressing replacement is required. It is convenient for treatment of different wound sites, with different shapes and sizes. They are not easy to be adhered to the wound bed. Form dressing is also easy to use with good compliance, and easy to tear off without hurting the skin. This dressing also has the ability of insulating, preserving heat, buffering external impulse/pressure, and prolonging the use time of wound dressing.
The disadvantages are that the external dressing is needed for the non-adhesive edge or to use two layers of dressing or adhesive tape. And it is opaque and the wound cannot be observed directly. Once large leakage happens or dressing replacement is delayed, it may cause skin around the wound impregnated. This dressing is not suitable for eschar or dry wounds.
Gauze dressings
Gauze dressings are made of braided or non-braided materials, mostly cotton, with multiple shapes and sizes (Table 1). Gauze is suitable for one-time use in cleaning, hemostasis bandaging or hygienic care of surgical or local wounds (Figure 2) [8,14]. It is helpful for wound infection, wound protection, wound exudate management. Gauze is actually useful for many kinds of wounds. They are easily available with low price. Gauze dressing can protect wounds and reduce bacterial invasion. It is cheap and suitable for various consumption levels. The disadvantages are that this type of dressing is required for frequent replacement that increases the total cost. And it may adhere to the wound bed. Gauze dressing often needs to be combined with other types of dressings; it cannot be used for wet wound healing. Their barrier functions are poor with high possibility of germ invasion. The granulation tissue of wound is easy to grow into the mesh eye of gauze. It will damage the newborn tissue and cause pain during dressing replacement. The sticky wound may cause not only pain but also secondary trauma during dressing replacement.
Composite dressings
Composite dressings are made of any kind of dressing materials, such as a combination of foam and gauze, alginate and silver ion dressing, alginate and carboxymethyl cellulose sodium(CMC). Composite dressings can be used as one-layer or two-layer dressing and for a variety of wound types [11,17]. This dressing is a new type of interactive wound-cleaning dressing. With its outer layer being a hydrophobic synthetic fiber material, the core part of which is polypropylene acid ester (SAP). SAP has a high affinity for proteins and can actively absorb wound exudates and necrotic tissues. Its indications are grade II burn wounds, small area grade III burn wounds, surgical wounds (such as skin necrosis after operation, treatment of infectious wounds), refractory chronic wounds (such as diabetic gangrene, deep pressure ulcer, refractory ulcer) [25]. Particularly, this dressing is good for debridement of rotten granulation wounds and old granulation wounds. Its advantages are easy to use with continuous debridement, accelerating necrotic tissue exfoliation, controlling germ infection and promoting wound healing [25]. There is effective protection of skin grafts in recipient areas to prevent infection and necrosis. Also, this dressing does not stick to the wound bed. Its disadvantages are higher price, lower cost performance and lower flexibility of indications. The dressings need daily replacement and are not suitable for wounds with vascular exposure on the wound surface, especially those with partial vascular embolism and necrosis.
Alginate dressings
The alginate dressings are composed of the extracts of natural brown algaemainly polysaccharide (Figure 2). They are braided or non-braided. These dressings have strong infiltration capacity and may become gelatinous after contacted with exudate fluid [17,18]. They can be used for the treatment of venous ulcer, sinus wound and severe exudate wound [10]. Their action mechanism is mainly through the exchange of sodium ions and water in wound exudates with calcium ions in alginate dressings, to make calcium alginate become gel, provide moist healing environment, promote cell proliferation at wound area, reduce pain, protect new tissue from injury and accelerate wound healing. Plus, macrophages are activated by fibrous stimulation of gel and calcium alginate, and further remove infectious tissue and scab crust, promote the release of growth factors, and promote the proliferation of fibroblasts and keratinocytes and accelerate healing. Alginates stimulate platelet adhesion/ agglutination, activate the intrinsic coagulation factors and further stop bleeding. Alginate dressings are applied to treat superficial wounds, wounds with skin removal, the wounds with medium to large amount of exudates, the wounds with holes and sinuses, the infectious wounds with necrotic tissue or cancerous wounds. Alginate dressings have strong absorptive capacity to absorb a large amount of infiltration. The ion exchange between sodium and calcium occurs after dressings contacting with exudate, which releases calcium ion and plays the role of hemostasis and stabilization of biomembrane. Dressings can form gel on wound bed and provide a wet healing environment to keep nerve endings moist, relieve pain, avoid dehydration and promote epithelial regeneration. These dressings can form hydrates with necrotic tissues to promote wound autolysis and debridement [18]. These dressings are also convenient to use and easy to remove, with no toxicity and no allergy. They can be used for infective wounds and non-adherent wounds, and they also promote autolysis debridement. However, these dressings need a second layer of dressing. They cannot be used for wounds with small amount of exudate and dry eschar wounds. Gel may not be distinguished from germ infection. It may cause dehydration and dry wound beds. These dressings misused to exposed tendons, key capsules or bones, may cause necrosis of these tissues.
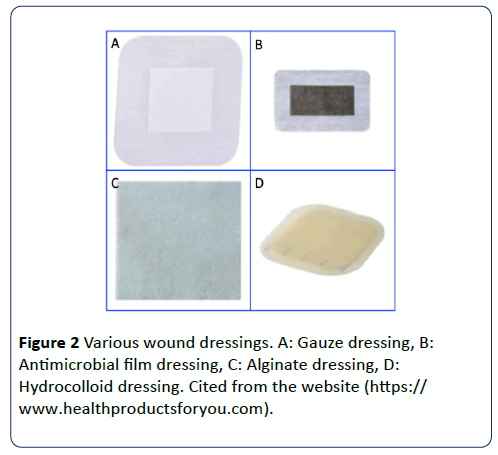
Figure 2: Various wound dressings. A: Gauze dressing, B: Antimicrobial film dressing, C: Alginate dressing, D: Hydrocolloid dressing. Cited from the website (https:// www.healthproductsforyou.com).
Hydrocolloid dressings
The ingredient of the hydrocolloid dressings (Figure 2) is mainly carboxymethyl cellulose sodium (CMC) [28]. Flake hydrocolloid is composed of CMC, hypoallergenic medical adhesive gel, elastomer and plasticizer. Its surface is a layer of semi-permeable poly membrane structure. The hydrocolloid dressings contain colloidal particles, such as gelatin or pectin, which can be transformed into gel-like substance when contacted with exudate. Thus, hydrocolloid dressings display certain exudate absorptive capacity, as well as having strong stickiness [6,13]. Hydrocolloid dressings can be used for venous ulcers, pressure sores, phlebitis, burns, etc. [12] and the dressings also are suitable for superficial wounds (such as superficial bedsore, small burns at small area, frictional wounds), wounds with a small to medium amount of exudate and wounds at skin removal sites [13]. Hydrocolloid dressings contain softening fibrinogen-softening components that can soften and remove fibrin. Meanwhile, they also contain hydrophilic particles that can interact with water to form gel membrane, further provide a wet environment and help reduce pain while not injuring newborn tissues. Hydrocolloid can activate macrophages and polymorphonuclear leukocytes to display their functions of autolysis debridement.
These dressings can keep the wound moist and hypoxic and slightly acidic environment, dissolve fibrinogen and accelerate autolysis debridement and wound healing [17]. These dressings have strong and fast absorptive capacity. They have the ability to absorb a small to medium amount of exudates. Dressings form gel to protect the exposed nerve endings, reduce pain and do not cause mechanical damage. They have moderate exudate absorption capacity and can promote autolysis debridement, close wound bed, protect wounds. They are waterproof and bacteriostasis, preventing urine and feces pollution, keeping insulation and moisturization, providing hypoxic and wet healing environment, supporting autolysis debridement. They are flake self-adhesive, without the second layer of dressing, to prevent germ invasion. After absorbing the exudates, they form gel and keep the nerve endings moist. They are non-adhesive to the wound bed and promote epithelial migration and granulation tissue growth. They are easily used and convenient with good compliance. But hydrocolloid dressings cannot be used for wounds with excessive exudates and infected wounds. Residues left in the wound bed may be misjudged for germ infection. These dressings also cannot be used for infectious wounds. After absorbing the exudates, the dressings will turn white locally, which may cause misunderstanding. They are strong sticky, the stickiness may cause skin damage. They are opaque and not easy to observe the wounds. They are easy to impregnate the skin. The change of dressings may affect the fragile skin around wounds.
Transparent membrane dressings
Transparent membrane dressings consist of polyester membrane, acrylic adhesive agents and other polymer materials [9,10]. The membrane is supported with a flexible lattice pad to make the dressings simple and convenient. They are semipermeable, allowing oxygen and water vapor to pass through, while preventing water and germ from passing through. These dressings are suitable for the treatment of superficial wounds, frictional wounds, skin-scratching wounds, skin donor sites or skin with external contamination [10,13]. This type of dressing is cheap and convenient and has good wound adhesion ability. They are good for autolysis debridement. They can prevent the wound bed friction and keep the wound bed moist and prevent germ contamination. Doctors can observe the wound situation without dressing removal. This type of dressing may adhere to certain wounds and are not easily removed off, and cannot be used for wounds with severe exudates. The dressing-sealed wounds may lead to impregnation of skin surrounding the wounds.
Hydrogel dressings
There are two types of hydrogel dressings including sheet dressing and amorphous dressing. Their main components are sodium carboxymethyl cellulose (CMC), pectin or propylene glycol [16,29]. Hydrogel dressings display weak exudate absorptive capacity due to having high water contents. However, they can actively provide water and moist environment for the dry wounds. The sheet hydrogel dressings are mainly used in the late stage of wound healing, such as epithelial stage, phlebitis, and exosmosis resulting from treatments of chemotherapeutic drugs. The amorphous hydrogel dressings are also known as debriding gel, which is mainly used for supporting autolysis debridement and softening wound eschar. Hydrogel dressings are commonly used in clinic [18,22]. Although there are different types of hydrogel dressings, their function and effect are basically similar with the major ingredients being slightly different [18]. The main mechanisms are that these dressings provide the wounds a moist environment and promote and activate polymorphonuclear leukocytes and macrophages in order to achieve the effect of wound autolysis debridement. This type of dressing is mainly suitable for wound autolysis debridement such as yellow rotten tissue and black necrotic tissues, wounds with small or moderate exudates, wounds from burns and radiation treatment, and wounds from exposed periosteum and tendon.
The advantages are that these dressings can hydrate the wounds to provide a moist environment, promote autolysis debridement for wound scab. They do not adhere the wound bed and they are easily removable with no pain and no wound damage [28]. They are conducive to epithelial migration and granulation growth. However, there are no germ barriers. This type of dressings is easy to cause skin immersion around wound and need a second layer of dressing in wound treatments, otherwise, possibly resulting in germ infection and contamination [5,25]. Thus, it is necessary and critical to develop new generation antimicrobial dressing. Meanwhile, these dressings are not suitable for wounds with large amount of exudates. Another disadvantage is high cost and more expensive.
Antibacterial wound dressings
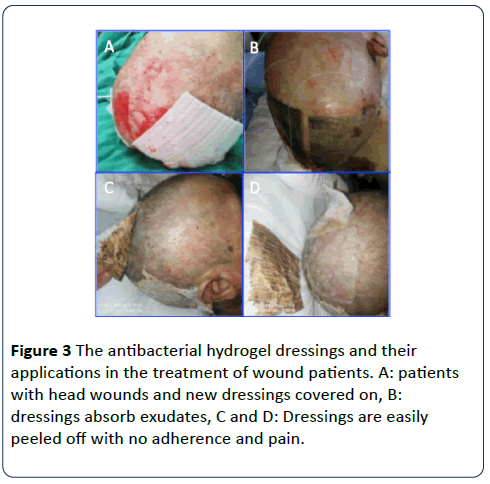
Wound healing and recovery is always associated with many aspects, particularly, the bacterial imbalance such as mixed germ infection and deep infection, and the long-lasting inflammatory response resulting from bacterial metabolites and necrotic tissues [4]. Thus, besides traditional functions, a good wound dressing with the prevention and protection of germ infection is very important in wound recovery. This type of antibacterial dressing as a new generation and broad-spectrum antimicrobial dressing has been developed (Figure 2) [5,18,22]. One of its key components is silver ion [30]. The dressings can continuously release silver ions. These positive charged silver ions are highly toxic to microorganisms, fungi and some viruses [30]. These silver ions can inhibit germ growth and achieve antimicrobial effects via stopping the synthesis of proteins on bacterial cell walls. The bacteria die due to cell wall fracture, and the bactericidal efficacy can be kept for 3-7 days. These antibacterial dressings are mainly suitable for serious contaminated wounds, infected wounds, diabetic foot ulcers, bedsores and other wounds [15,25,29]. Once the silver ions are combined with other dressings that can absorb exudates, these dressings display their ability to prevent and treat various local infections [31]. The range of germ inhibition is gram-positive, gram-negative bacteria, vancomycin-resistant Enterococcus and Candida albicans [26]. Silver-containing hydrophilic dressings such as Aquacel Ag extra hydrogel consist of sodium carboxymethyl cellulose (CMC-Na) and 1.2% silver ion [22,28] (Figure 3). These dressings can be used to treat primary healing wounds and act as an effective barrier to prevent germ penetration.
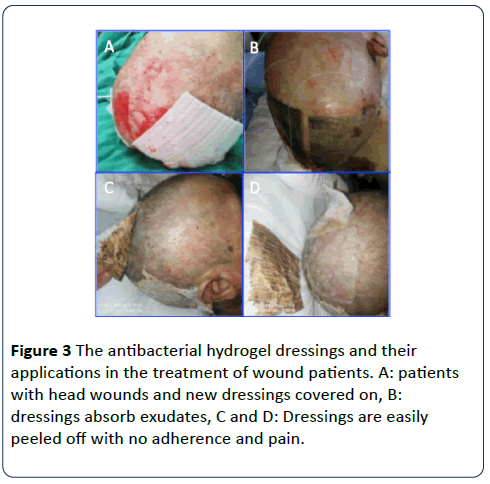
Figure 3: The antibacterial hydrogel dressings and their applications in the treatment of wound patients. A: patients with head wounds and new dressings covered on, B: dressings absorb exudates, C and D: Dressings are easily peeled off with no adherence and pain.
Conclusion
Although there are so many different types of wound dressings, especially, we made a great progression in antibacterial wound dressings. However, these dressings are still not competent and satisfied. For example, these hydrogel dressings are easily peeled off and convenient, but they have low exudate absorptive capacity. Dressings containing silver ions can kill germs and reduce wound infection, but silver ions are toxic when wounds are exposed to them too long time or dressings contain high concentration of these ions [31]. Patients may also be silver-allergic and cannot use these dressings. Thus, it is a need to develop novel wound dressings. By keeping the advantages of the traditional dressings, these novel dressings may have more nutrients for wound recovery, high exudate absorptive capacity, or antibacterial and safe peptides instead of toxic silver ions. We are attempting to develop hydrogel dressing with antibacterial peptides, avoiding or reducing the use of silver ions. Meanwhile, a good quality and affordable dressing is also expected and needed.
Acknowledgement
This work was supported by the Natural Science Foundation of Hunan Province (2007JJ6052), Zhishan Plan Program of the Third Xiangya Hospital, Central South University (2017/15), Xiangtan Institute of Industrial Technology Collaborative Innovation and Xiangtan Science and Technology Bureau.
24605
References
- Kangal OMK, Regan JP (2018) Wound healing in Stat Pearls. Treasure Island (FL).
- Young AW, Dewey WS, King BT (2019) Rehabilitation of burn injuries: an update. Phys Med Rehabil Clin N Am 30: 111-132.
- Guest JF, Ayoub N, McIlwraith T, Uchegbu I, Gerrish A, et al. (2017) Health economic burden that different wound types impose on the UK's National Health Service. Int Wound J 14: 322-330.
- Sulaeva I, Henniges U, Rosenau T, Potthast A (2015) Bacterial cellulose as a material for wound treatment: Properties and modifications. A review. Biotechnol Adv 33: 1547-1571.
- Davis SC, Li J, Gil J, Valdes J, Solis M, et al. (2018) The wound-healing effects of a next-generation anti-biofilm silver Hydrofiber wound dressing on deep partial-thickness wounds using a porcine model. Int Wound J 15: 834-839.
- Xie G, Zhang F, Li S (2017) The effect of foam dressing combined with hydrocolloid dressing on the treatment of stage III and IV compression chambers. Chongqing Medical 27: 3-10.
- Zhang X, Sun D, Jiang GC (2018) Comparative efficacy of nine different dressings in healing diabetic foot ulcer: A Bayesian network analysis. J Diabetes 11: 418-426.
- Kaushik D, Joshi N, Kumar R, Gaba S, Sapra R, et al. (2017) Negative pressure wound therapy versus gauze dressings for the treatment of contaminated traumatic wounds. J Wound Care 26: 600-606.
- Gomez-Rodriguez GH, Lopez-Mata MA, Valbuena-Gregorio E, Melchor RGV, Campos-Garcia JC, et al. (2018) Microencapsulation of carvacrol using pectin/aloe-gel as a novel wound dressing films. Curr Top Med Chem 18: 1261-1268.
- Ahmed A, Boateng J (2018) Calcium alginate-based antimicrobial film dressings for potential healing of infected foot ulcers. Ther Deliv 9: 185-204.
- Chen Y, Qiu H, Dong M, Cheng B, Jin Y, et al. (2019) Preparation of hydroxylated lecithin complexed iodine/carboxymethyl chitosan/sodium alginate composite membrane by microwave drying and its applications in infected burn wound treatment. Carbohydr Polym 206: 435-445.
- Cortes OL, Salazar-Beltran LD, Rojas-Castaneda YA, Alvarado-Muriel A, Serna-Restrepo A, et al. (2018) Use of hydrocolloid dressings in preventing pressure ulcers in high-risk patients: a retrospective cohort. Invest Educ Enferm 36: e11.
- Dutra RA, Salome GM, Leal LM, Alves MG, Moura JP, et al. (2016) Cost comparison of pressure ulcer preventive dressings: hydrocolloid dressing versus transparent polyurethane film. J Wound Care 25: 635-640.
- Ma Y, Zhang H, Zhu X, Chen W, Chen X, et al. (2018) Clinical application of polyamide gauze dressing in acute and chronic wounds. Chinese General Medicine 3: 4-10.
- Yi Z, (2017) Report on the effect of combined treatment of foam dressing and silver ion alginate dressing on stage IV nursing. Chinese J Metallurgical Industry Med 4: 2-8.
- Jiang Y, Liu X (2017) Application of hydrocolloid dressing in skin abrasion dressing. Chinese J Med Clin Med 31: 3.
- Re C, (2017) Current situation and prospect of medical dressing research. Chemical Industry 8: 2-8.
- Bradford C, Freeman R, Percival SL (2009) In vitro study of sustained antimicrobial activity of a new silver alginate dressing. J Am Col Certif Wound Spec 1: 117-120.
- Widgerow AD (2015) The burn wound exudate-an under-utilized resource. Burns 41: 11-17.
- Tiwari VK (2012) Burn wound: How it differs from other wounds? Indian J Plast Surg 45: 364-373.
- Suzuki K, Birnbaum Z, Lockhart R (2017) Skin perfusion pressure and wound closure time in lower extremity wounds. J Am Coll Clin Wound Spec 9: 14-18.
- Ip M (2006) Antimicrobial activities of silver dressings: an in vitro comparison. J Med Microbiol 55: 59-63.
- Shaik MM, Dapkekar A, Rajwade JM, Jadhav SH, Kowshik M (2019) Antioxidant-antibacterial containing bi-layer scaffolds as potential candidates for management of oxidative stress and infections in wound healing. J Mater Sci Mater Med 30: 13.
- Park JK, Lee JH, Kwak JJ, Shin HB, Jung HW, et al. (2013) Evaluation of an antimicrobial silver foam dressing. Wounds 25: 153-159.
- Zmejkoski D, Spasojevic D, Orlovska I, Kozyrovska N, Sokovic M, et al. (2018) Bacterial cellulose-lignin composite hydrogel as a promising agent in chronic wound healing. Int J Biol Macromol 118(Pt A): 494-503.
- Percival SL, Thomas J, Linton S, Okel T, Corum L, et al. (2012) The antimicrobial efficacy of silver on antibiotic-resistant bacteria isolated from burn wounds. Int Wound J 9: 488-493.
- Huang X, Ni X (2016) Nursing experience of applying dressing for III, IV degree and non-staged pressure storage. Chinese Med Sci 24: 4-11.
- Liang M, Chen Z, Wang F, Liu L, Wei R, et al. (2018) Preparation of self-regulating/anti-adhesive hydrogels and their ability to promote healing in burn wounds. J Biomed Mater Res B Appl Biomater 107: 1471-1482.
- He O (2015) Sulfadiazine silver lipid hydrogel dressing for the treatment of small area skin defects and wound infection. China Tissue Eng Res 21: 4-10.
- Walker M, Parsons D (2014) The biological fate of silver ions following the use of silver-containing wound care products - a review. Int Wound J 11: 496-504.
- Wilkinson LJ, White RJ, Chipman JK (2011) Silver and nanoparticles of silver in wound dressings: a review of efficacy and safety. J Wound Care 20: 543-549.