Keywords
Compliance; Hypertension; Survey; Clinician; HCPs
Key Messages
Indian clinicians’ viewpoint is that the non-compliance to the medication is one of the major modifiable risk factor for the management of uncontrolled hypertension.
Introduction
Hypertension (HTN) is a vital public health challenge in both economically developing and developed countries. It is one of the crucial risk factors for cardiovascular mortality [1]. Worldwide cardiovascular disease accounts for approximately 17 million annual deaths which is just about one third of the total deaths. Of these, complications of hypertension account for 9.4 million deaths worldwide every year [2]. About 54% of stroke and 47% of ischemic heart disease worldwide are attributable to high blood pressure [1]. Hypertension is the leading modifiable risk factor for cardiovascular diseases and was the topmost leading risk factor for global disease burden in 2010 [3]. The situation is critical in the South heat Asian region with studies reporting HTN as an important risk factor for the attributable burden of disease in the region. An alarming rise in HTN projected by the Global Burden of Hypertension 2005 study and a systematic analysis for the GBD (Global Burden of Disease) 2010 by Limm et al. portrays a gloomy picture for the Indian population [1]. Recent meta-analysis by Anchala et al. found that about 33% urban and 25% rural Indians are hypertensive [4].
To reduce the risk of cardiovascular disease, hypertensive patients must be treated appropriately, either through lifestyle interventions alone or in combination with medication [5]. It is generally believed that, anti-hypertensive medications are effective in reducing high blood pressure and have been shown to significantly reduce the risk of cardiovascular illness [6]. In spite of availability of multiple drugs with good efficacy and few side effects for the treatment of hypertension, rate of blood pressure control is disappointing [7]. The uncontrolled hypertension includes patients who lack blood pressure control secondary to poor compliance and/or an inadequate treatment regimen, as well as those with true treatment resistance [8]. Around 54% of diagnosed Caucasian patients of hypertension are not under control [9]. For Asian patients, the proportion of patients whose blood pressure remains uncontrolled is even higher that is more than 70% [9].
Adherence is defined as ‘The extent to which the patient’s behaviour matches agreed recommendations from the prescriber’. It has been adopted by many as an alternative to compliance, in an attempt to emphasize that the patient is free to decide whether to adhere to the health care physician’s (HCP) recommendations and that failure to do so should not be a reason to blame the patient [10]. Poor adherence or compliance to therapies has been linked to a variety of problems, including poor blood pressure control, rehospitalisation, and increased healthcare resource utilization [11].
Most of the existing literature related to hypertension management focuses exclusively on patients and sheds little light on health care physicians’ (HCPs) perception on medication adherence that is likely to influence poor patient outcomes. Yet published literature conducted elsewhere suggests that physicians and patients differ substantially in their perceptions, knowledge, and/or attitudes which may lead to conflict or poor patient outcomes [12]. Accordingly, a better understanding of physicians’ viewpoint is needed to improve hypertension management and improve quality of care. The purpose of the current study was to capture HCP’s viewpoint on the therapy compliance in the management of hypertension.
Subjects and Methods
A cross-sectional survey of health care physicians (HCPs) treating hypertension like primary care physicians, consulting physicians, cardiologists and diabetologists was conducted. A convenience sample of HCPs working in government or private practice across the India was included for the survey. The paper-based survey was administered to all HCPs during a personal meeting with the study interviewer. With the intent to have the highest response rates in HCP groups, the survey was distributed on-site, and providers were requested to complete and return it personally in hand to the interviewer.
The survey instrument (Paper based questionnaire) was developed by researchers upon review of existing literature and detailed discussion with the few practicing clinicians. Face and content validity along with reliability (test-retest method) was assessed through a focused panel of HCPs to determine if content was adequate to obtain the necessary data. In doing so, information on redundancies and inaccuracies were identified and corrected. The same panel of HCPs was provided the survey again after due correction and was finalized accordingly. The data collection was performed internally by the trained interviewers throughout the period of May-July 2016.
The survey questionnaire is represented in the Appendix at the end. Response anchors to each question were incorporated in the questionnaire and an option for capturing additional comments was also included. Here, according to the need and appropriateness, likert scale was used for valid quantification of the clinicians’ view.
Based on their clinical experience, HCPs were asked to estimate the percentage of their patients who were not controlled for their hypertension. Accordingly, they were also asked to pick reasons for uncontrolled hypertension like compliance to the medication and safety and efficacy of medicine categorically. Here, the WHO definition of compliance/adherence was provided, which is taking a medication at least 80% of the time. Further they were asked to give order to the certain factors according to their clinical experience, which affect patient compliance and may cause uncontrolled hypertension. In addition, Physicians were asked to put a figure on their patients (<25%, 25%-49%, 50%-75%, and >75%) according to commonly used excuses for the noncompliance to the medication by patients. At last they were asked about their view on the patient compliance program and other corrective measures like daily dose reminder, patient education etc. to tackle the non-compliance to the medication in hypertension.
Results
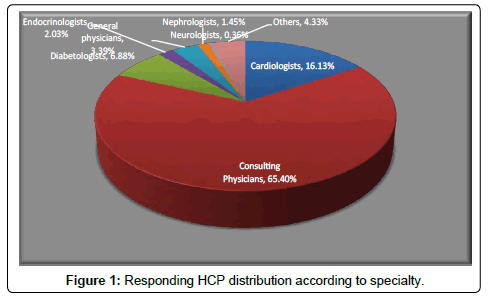
Total 2746 HCPs responded to this paper based questionnaire. This survey was conducted across the India covering more than 150 cities. Here, greater part of responding HCPs was found to be consulting physicians. Find below (Figure 1) the specialty wise distribution.
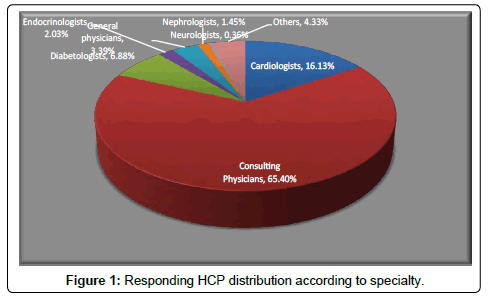
Figure 1: Responding HCP distribution according to specialty.
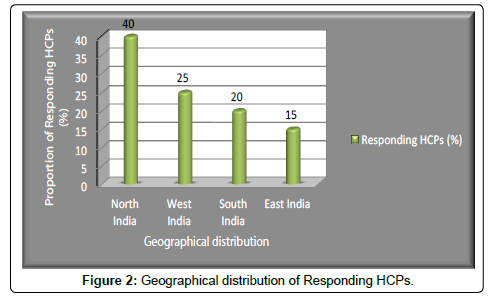
Response rate for the individual question was varied among physicians within the range of 88%-99%. Geographical distribution of responders was more in favour of North India which was followed by West, South and West (Figure 2).
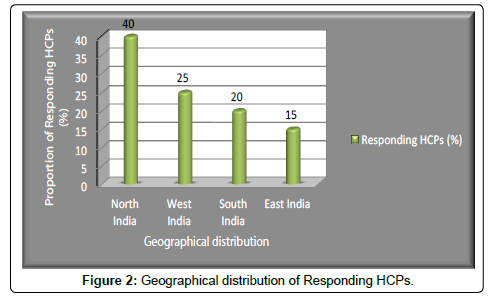
Figure 2: Geographical distribution of Responding HCPs.
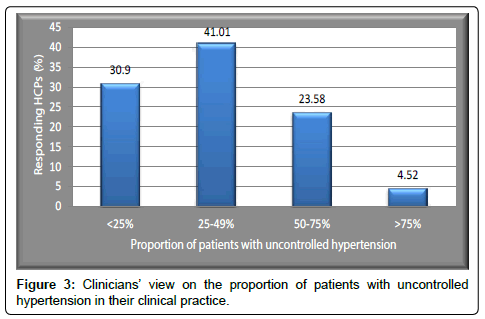
Out of total responders 28.10% out of responders expressed that ≥ 50% of hypertensive patients in their individual health care setting are having uncontrolled hypertension. Further to this approximately 69% of clinicians believed that more than 1/4th of their patients can be categorized as uncontrolled hypertensive (Figure 3).
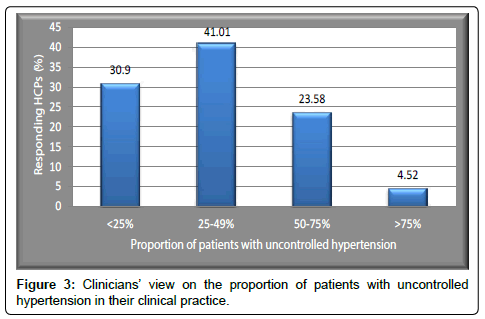
Figure 3: Clinicians view on the proportion of patients with uncontrolled hypertension in their clinical practice.
Greater part of responding HCPs, around 47%, felt that noncompliance to the medication is the reason for not obtaining blood pressure control in around 25-50% of their uncontrolled hypertension patients. Again around 2/3rd (66%) of our responders put noncompliance as the reason for uncontrolled hypertension in >25% of their patients who are not controlled for BP. This number was numerically more when we compared the same category for other two reasons, safety (tolerability) of the medicine and efficacy (effectiveness) of the medicine, for the uncontrolled hypertension (Figure 4). Majority of clinicians also expressed that patient related factors are principally responsible for the non-compliance to the medicine.

Figure 4: Responding HCPs stating reasons for uncontrolled hypertension.
Simultaneously HCPs were asked to quantify (level of agreement) their viewpoint in the context of patient related factors (responsible for uncontrolled hypertension) like noncompliance to the medicine, noncompliance to the lifestyle modifications and unawareness of disease by patients. Out of all responders, staggering 93.5% were in agreement that non-compliance to the medicine is a major reason for the uncontrolled hypertension and around 45.4% even strongly agreed to this. Non-compliance to lifestyle modification and disease unawareness by patients also contribute to uncontrolled hypertension, this was felt by approximately 88% and 80% of HCPs respectively.
When HCPs were asked about patient reported reasons for not complying with therapy, their opinions were almost uniformly distributed for all categories. Here, more than half (~55%) of our responders felt that 25% or more of their patient’s stat forgetfulness as the reason for non-compliance. While 60%, 71.6% and 71% clinicians said reasons like I am afraid of side effect, cost of medicine and polypharmacy respectively are given by more than 1/4th of their patients (Figure 5).

Figure 5: HCPs view on patient reported reasons for the non-compliance to the therapy (For more than 1/4th of their patients).
When HCPs were asked about various measures to improve the compliance of patients to the antihypertensive medications, they consider all factors like daily dose reminder, patient education program and low cost of medicines important. Here, patient education program came out as the preferred option (38%) followed closely by low cost of the therapy and daily dose reminder.
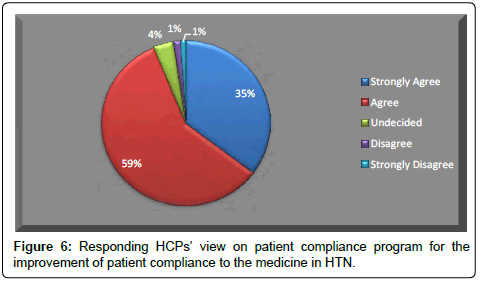
Doctors were also asked to opine their agreement related to importance of robust patient compliance program for the improvement of patient compliance for antihypertensive medications. Around 94% of responders were in the agreement that patient compliance program can improve the compliance to the medicine in hypertension management. Further to this 35% physicians strongly agreed to this. Only 2% of responders disagreed to the said program for the improvement of compliance (Figure 6).
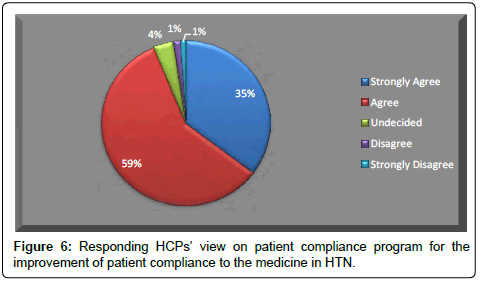
Figure 6: Responding HCPs view on patient compliance program for the improvement of patient compliance to the medicine in HTN.
When doctors were administered a specific question about the place of dose reminder services (daily dose reminder and monthly repurchase reminder) in the patient compliance program, majority of them (85.5%) were in agreement that patient should be enrolled in such reminder services (Figure 7).

Figure 7: HCPs view on dose reminder services for the improvement of patient compliance to the medicine in HTN.
Discussion
In the context of arterial hypertension, a chronic disease that requires lifestyle interventions and pharmacotherapy for life, the major challenge makes itself known: the adherence to the therapy as a subjective construct to be measured. Further to this when it comes to measure subjective response from clinicians regarding the patient behaviour, it becomes more challenging to create an objective modality. Here in we developed a brief survey questionnaire to map the clinicians’ view regarding the issue and solution of hypertension, pertaining in particular to treatment compliance.
Our study findings suggest that majority of clinicians (41%) felt that 25-50% of their patients of hypertension are not controlled for their blood pressure. While 30% of responders expressed that <25% of their patients are not under control for the hypertension. The recent meta-analysis by Anchala et al. [4], for the prevalence, awareness, and control of hypertension in India, suggested that around 20% of urban hypertensive patients who are taking medications are not under control. This difference may draw attention to the disparity in clinicians’ perception and actual scenario as far as control of hypertension is concerned.
Now it is a known fact that pharmacological antihypertensive therapy has a positive safety and tolerability profile and it reduces the risk of stroke and myocardial infarction (MI). But available evidence suggests a divergent trend, as many as 50% to 80% of patients treated for hypertension are non-adherent to their treatment regimen [13]. In our study, around 66% of our responders put non-compliance as the reason for uncontrolled hypertension in more than ¼th of their patients. Majority of HCPs also expressed that patient related factors are principally responsible for the non-compliance. Further to this, more than 90% of our responders were in agreement that non-compliance to the prescribed medicine is a major patient related factor for not having desired control of the blood pressure. This clearly delineates the pervasiveness of bothersome issue, non-compliance to the medications, in hypertension management. Medication compliance continues to decline even after a catastrophic event such as a stroke [14]; thus, it is not startling that treating asymptomatic conditions like hypertension to prevent the possible occurrence of adverse consequences years later presents an even greater challenge.
Forgetfulness by the patient is a widely reported factor that causes non-compliance with medication or clinic appointments [15]. Confirming this, in our survey more than half (~55%) of our responding HCPs felt that 25% or more of their patients gives forgetfulness as the reason for non-compliance. These findings pave the way for the identification for certain solutions to tackle the rising issue of noncompliance.
The multi-factorial nature of poor medication adherence implies that only a persistent, coordinated effort will guarantee optimal medication adherence and realization of the full benefits of current therapies. When HCPs were asked about the measures to improve the compliance of patients to the antihypertensive medications, they consider all factors like daily dose reminder, patient education program and low cost of medicines important. More than 90% of responders were in the agreement that a consolidated compliance program encompassing all these factors can improve the compliance to the medicine in hypertension management. Additionally, when HCPs were asked a specific question about the place of dose reminder services (daily dose reminder and monthly repurchase reminder) in the patient compliance program, majority of them (85.5%) were in agreement that patient should be enrolled in such reminder services.
There are some limitations to this study. The sample size may not have been large enough to demonstrate accurate generalized extrapolation. But it should be sufficient enough to understand the magnitude of the problem in hand, non-compliance to antihypertensive medication. However, clinicians who were willing to participate in interviews and focus groups may not be representative of the general clinical fraternity. We do not believe there is any reason our findings would not be relevant to Indian physicians and patients both in general, including those not represented in this study. Although clinicians’ view on non-compliance to the medications was not quantified in this survey per se, its correlation with the actual outcome (uncontrolled hypertension) was tried to address appropriately.
These findings may have vast public health significance for strategy makers and physicians alike. The low treatment and medication adherence levels among hypertensive patients signify a lower knowledge, attitude, and practice levels among patients. Current strategies to control BP among Indian hypertensive patients may not be working because less utilization of prescribed medication.
Conclusion
Indian clinicians feel that uncontrolled hypertension is still be a widely prevalent problem in spite of availability of effective antihypertensive drugs and non-compliance to the medication is one of the major modifiable risk factor for this. This warrants the development of strategies for the improvement of compliance at the grassroots level focusing on patient behaviour and education.
Conflict of interest
All authors are full time employee for Intas Pharmaceuticals Limited, Ahmedabad, India.
Acknowledgment
We would like to acknowledge the support provided by Dr. Dixit Patel, Dr. Hiren Prajapati, Dr. Kamlesh Patel, Mr. Daxesh Patel & Mr. Aakash Goyal during the conduct of a study and review of a manuscript.
20401
References
- Kishore J, Gupta N, Kohli C, Kumar N (2016) Prevalence of Hypertension and Determination of Its Risk Factors in Rural Delhi. Int J Hypertens e7962595.
- Doulougou B, Gomez F, Alvarado B, Guerra RO, Ylli A, et al. (2016) Factors associated with hypertension prevalence, awareness, treatment and control among participants in the International Mobility in Aging Study (IMIAS). J Hum Hypertens 30: 112-119.
- Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, et al. (2014) Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens 32: 1170-1177.
- Meinema JG, Van DN, Beune EJAJ, Jaarsma DADC, van Weert HCPM, et al. (2015) Determinants of Adherence to Treatment in Hypertensive Patients of African Descent and the Role of Culturally Appropriate Education. PLoS One 10: e0133560.
- Kamran A, Sadeghieh Ahari S, Biria M, Malepour A, Heydari H (2014) Determinants of Patient’s Adherence to Hypertension Medications: Application of Health Belief Model Among Rural Patients. Ann Med Health Sci Res 4: 922-927.
- Pickering TG (2001) Why are we doing so badly with the control of hypertension? Poor compliance is only part of the story. J Clin Hypertens Greenwich Conn 3: 179-182.
- Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, et al. (2008) Resistant Hypertension: Diagnosis, Evaluation, and Treatment aScientific Statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 51: 1403-1419.
- Rahman ARA, Wang JG, Kwong GMY, Morales DD, Sritara P, et al. (2015) Perception of hypertension management by patients and doctors in Asia: potential to improve blood pressure control. Asia Pac Fam Med 14:2.
- Concordance, adherence and compliance in medicine taking (2005) Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO).
- Frishman WH (2007) Importance of medication adherence in cardiovascular disease and the value of once-daily treatment regimens. Cardiol Rev 15:257-263.
- Iwelunmor J, Blackstone S, Gyamfi J, Airhihenbuwa C, Plange-Rhule J, et al. (2015) A Concept Mapping Study of Physicians’ Perceptions of Factors Influencing Management and Control of Hypertension in Sub-Saharan Africa. Int J Hypertens,ID: e412804.
- Brown MT, Bussell JK (2011) Medication Adherence: WHO Cares? Mayo Clin Proc 86: 304-314.
- Glader EL, Sjölander M, Eriksson M, Lundberg M (2010) Persistent use of secondary preventive drugs declines rapidly during the first 2 years after stroke. Stroke J Cereb Circ 41: 397-401.
- Jin J, Sklar GE, Min Sen Oh V, Chuen Li S (2008) Factors affecting therapeutic compliance: A review from the patient’s perspective. Ther Clin Risk Manag 4: 269-286.