Keywords
bacterial colonization, cord care, cord separation time, ethanol, human breast milk
Introduction
Umbilical cord infections contribute to the increased morbidity and mortality in newborns of developing countries, where infants are exposed to unhygienic practices. The world health organization (WHO) estimates that 4 million children die each year during the neonatal period, with most deaths occurring in developing countries. Importantly, infections are the most common cause of neonatal mortality with approximately 1 million newborn dying annually worldwide from umbilical cord bacterial infections [1,2]. After delivery, the umbilical cord serves no purpose. The necrotic tissue of the umbilical cord is a potential site for infection [3] immediately after birth by bacterial contaminants [4]. Bacterial coloniza tion from cord stump infection is a factor that increases the morbidity and mortality of infants in developing countries [5]. Preventive umbilical cord treatments to reduce infection were introduced in the 1950’s and 60’s [6]. In developed countries, individual cases of umbilical cord infections continue to occur in aseptic nurseries [7]. Umbilical cord treatment after birth is a subject of research. A wide variety of cultural practices and beliefs are associated with umbilical cord care, which include topical application of human milk. Several reports show that the application of topical antiseptics increases the time to cord separation compared to dry cord care or non antiseptic treatment [8-13]. The hospital cost of umbilical cord treatment varies with the method of application and length of hospital stay. Therefore, it is important to find inexpensive alternative cord care; e.g. breast milk; in low socio-economic countries.
Controversial data about antiseptics and economic concerns has prompted a movement towards dry cord care [14-16], which is the current recommendation of the WHO for developing countries under routine circumstances [17]. However, WHO acknowledges the use of antiseptics when harmful, unhygienic, traditional practices in newborns increase the risk for omphalitis. Although there is no cost of natural cord drying, costs could be increased due to infections and expensive bacterial culture examinations. Several agents; including human breast milk; are used for umbilical cord care and their effect on cord separation time has been examined [5,18]. Breast milk is available, easy to use, and non invasive method for cord care. There is limited data that examined the effect of human breast milk topical application on bacterial colonization of umbilical cord stump. This study examines the effect of breast milk on cord separation time and bacterial colonization and compares it to that of 70% ethanol.
Subjects and Methods
Subjects and design
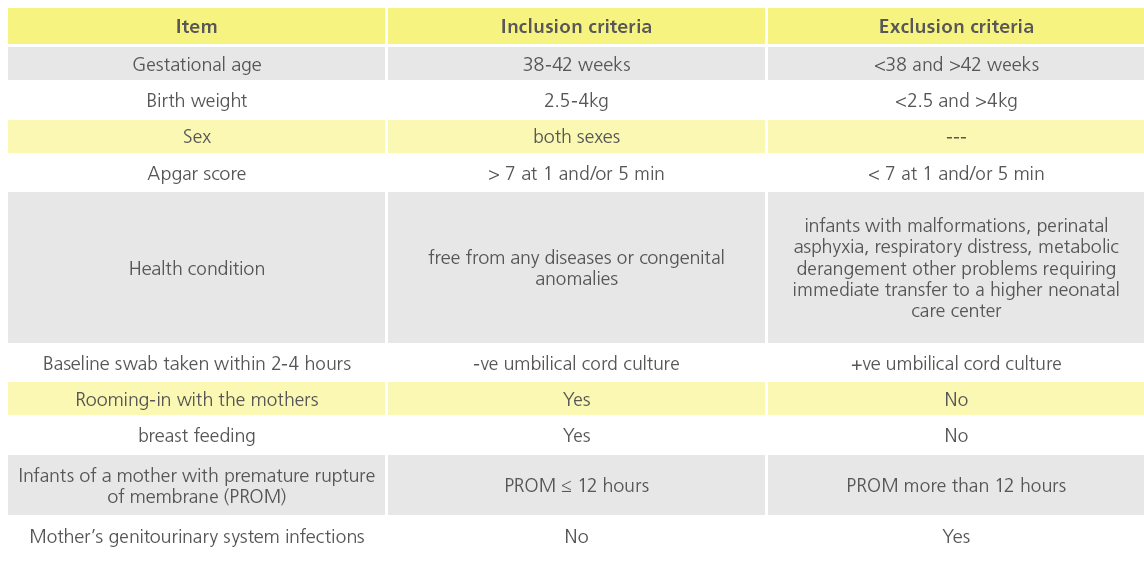
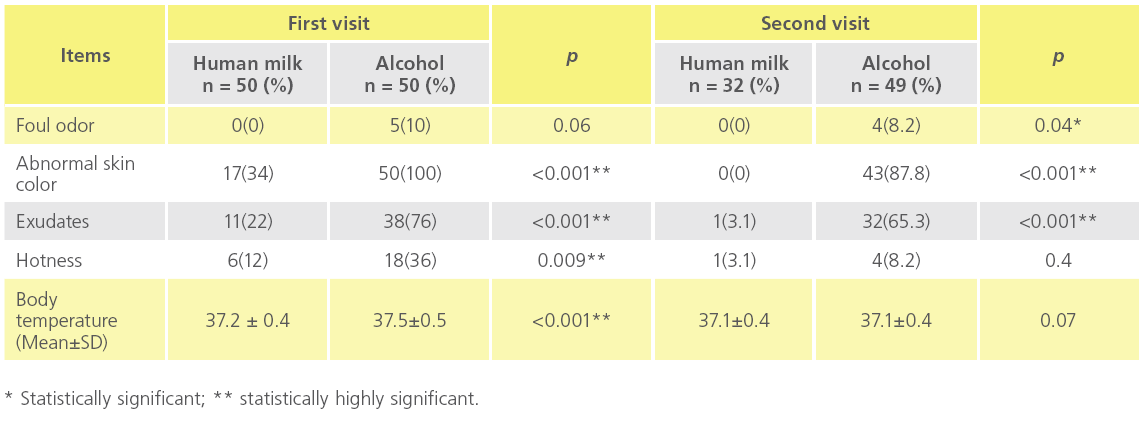
A quasi-experimental design (a design that lacks random assignments) was used and samples from 100 newborn infants were included in this study. The neonates were classified into two groups for studying the effect of human breast milk and 70% ethanol application on umbilical cord separation time, omphalitis and bacterial colonization (50 neonates in each group). The study protocol was approved by the local institutional review board at Minia University Hospital (MUH). An informed consent was obtained from the mothers prior to participation in the study. Inclusion criteria included babies followed immediately after birth with umbilical cord cut and clips applied according to MUH policy for immediate care of newborns. Summary of inclusion and exclusion criteria are shown in Table 1.
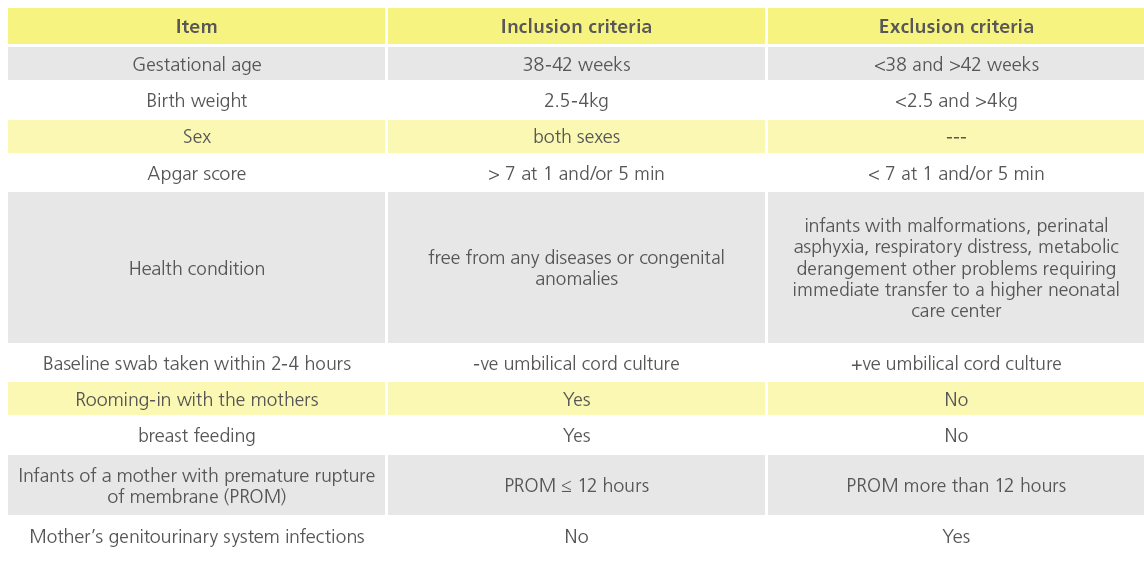
Table 1: Inclusion and exclusion criteria of the study subjects.
The neonates were assigned to receive one of the two regimens for umbilical cord care, namely breast milk or 70% ethanol. Group 1 neonates (n = 50) were treated with 2-3 drops of own mother’s milk (study group), while Group 2 neonates (n = 50) were treated with 70% ethanol (control group). Mother’s of each study group applied human milk or ethanol topically three times daily (every 8 hours) to the umbilical stump until two days after cord separation. In the breast milk study group, mother was instructed to wash hands and breasts, and then apply milk on the umbilical stump. This was applied 2-4 hours after birth (after taking a baseline umbilical cord swab for bacterial examination), thereafter every 8 hours and when needed. Mothers were instructed to retain milk on stump until dry and not to wash it out. All mothers were given a follow up leaflet before being discharged from the hospital with details of signs and symptoms of omphalitis, sepsis, cord separation time, time of breast milk daily application on the umbilical cord and time of follow up in the neonatology clinics at MUH. The observations related gross signs of omphalitis (inflammation of the umbilical cord region) include redness, swelling, exudates, hotness and odor were examined by naked eye and recorded three times (at the time of each swab collection) as previously described [17,19]. The mothers were instructed to record the umbilical cord separation time/date.
Methods
A baseline umbilical cord swab was taken from the base of the cord 2-4 hours after birth and immediately sent to the bacteriology laboratory. All specimens were labeled with the newborn’s name, code and date. The specimens were collected by a dry sterile swab soaked in Amies transport medium (Oxiod, England) for culture within 1-2 hours. Samples were serially diluted and cultured on blood- and MacConkey’s agar plates and incubated for 24-48 hours at 37oC. Those showing no bacterial growth at the baseline swab were microbiologically followed by two additional cord swabs. The first swab was collected on the 3rd day after birth and the second swab was collected at the day of cord separation. Every sample was cultured on MacConkey’s agar (Oxoid), and blood agar (Difco, UK) plates at one log serial dilutions of the specimen. Briefly, a 100ml was thoroughly smeared on each plate under aseptic conditions, and then incubated over night at 37oC until finally counted using an illuminated Fisher colony counter (Fisher, USA). The total viable count (TVC) on MacConkey’s or Blood agar plates was determined by taking the average of two counts on each of the two plates that were run at least in duplicates.
Statistical analysis:
Data were analyzed using the Statistical Package for Social Science (SPSS) version 13 (SPSS Inc. Chicago, IL) Numerical data were expressed as the mean and standard deviation (SD) while qualitative data were expressed as frequency and percentage. For quantitative data, comparison between two variables was done using student’s t-test while Fisher’s exact test was used for comparison of non parametric data. Probability (p-value) less than 0.05 was considered significant and less than 0.01 was considered highly significant.
Results
Socio-demographic data of the study subjects
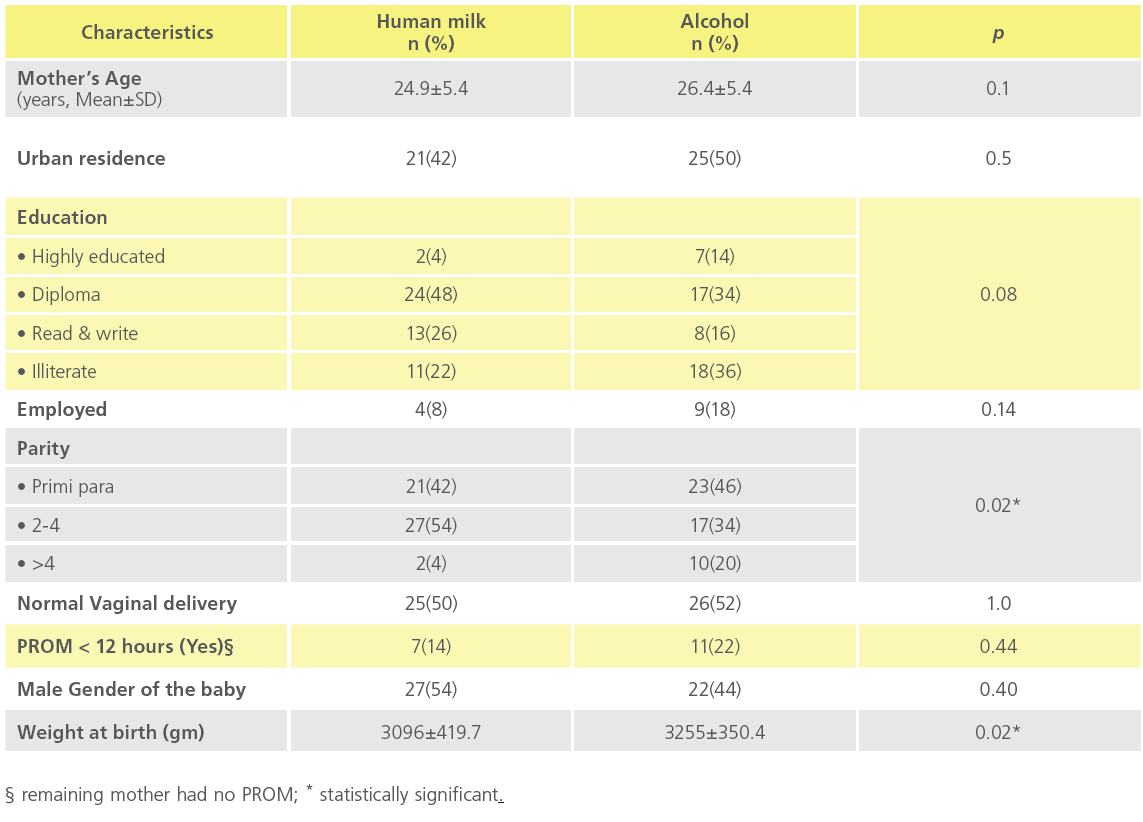
This study was conducted at MUH in the period from August 2009 to February 2010. Table (2) shows the socio-demographic characteristics of the mothers in the human milk and alcohol treated groups. The mean age of the mothers in the human milk and alcohol groups was 24.9±5.4 and 26.4±5.4 years, respectively. The alcohol group mothers were evenly split between urban and rural residence while only 42% of the mothers in the human milk group were urban residents (p=0.5). The majority of both groups were house wives (92% and 82% in the human milk and alcohol groups, respectively, with the remaining mothers being employed (p=0.14). Also, the differences between both groups in the educational level of the mothers (p=0.08), mode of delivery (p=1), and gender of the baby ((p=0.4) were all insignificant. On the other hand, a significant difference in distribution of parity status was found between the two groups (p=0.02). Although a significant difference was found among human milk and alcohol groups regarding the gestational age (not shown) and birth weight (p=0.02), these differences were within the normal ranges (Table 2) as the inclusion criteria include subjects with a wide range of gestational age (38-42 weeks) and normal birth weight (2.5-4.0 kg).
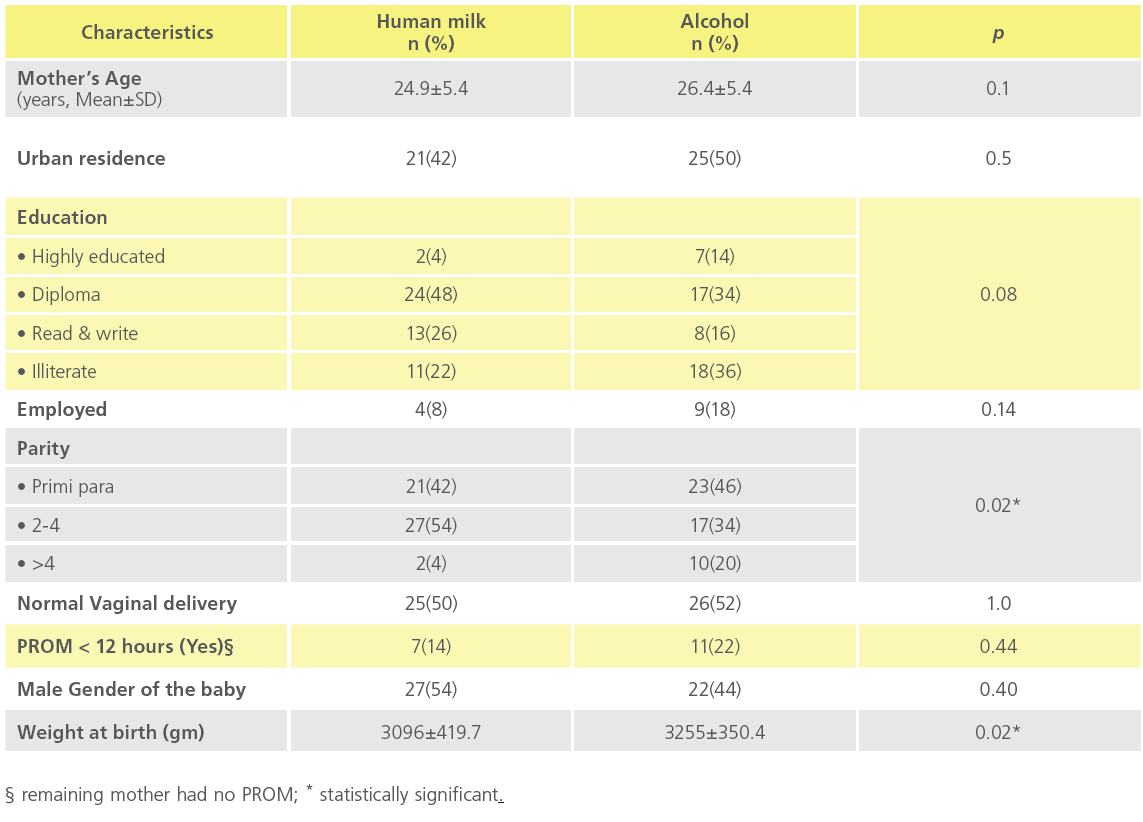
Table 2: Comparison between socio-demographic data of the mothers and neonates among human milk and alcohol groups (n = 50 each).
Human breast milk accelerates the umbilical cord separation compared to 70% ethanol:
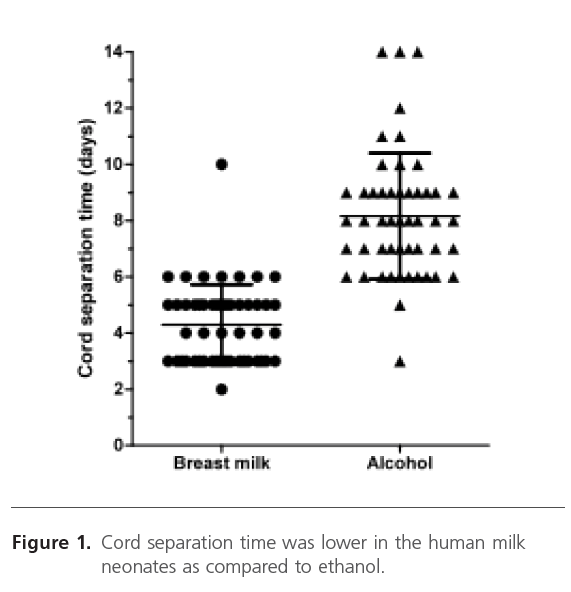
Figure (1) shows that cord separation was faster in the human milk neonates than in the alcohol group. In this regard, almost half of human milk group babies had their cord fallen off at the 3rd-4th day of age and 23 (46%) of them had their cord fallen off at the 5th-6th day of age. On the other hand, only 11 (22%) of the babies in the alcohol group had their cord fallen off at the 5th-6th day of age while the rest of the group had their cord fallen off at the 7th-8th reaching up to 10 days after delivery. Only one baby in the ethanol group had his cord falling at the 3rd day (Figure 1). The mean cord separation time was 4.3±1.4 and 8.16±2.2 in the human milk and ethanol groups, respectively. These data show that the mean cord separation time in the human milk group was significantly shorter (p <0.001) than in the alcohol group neonates.
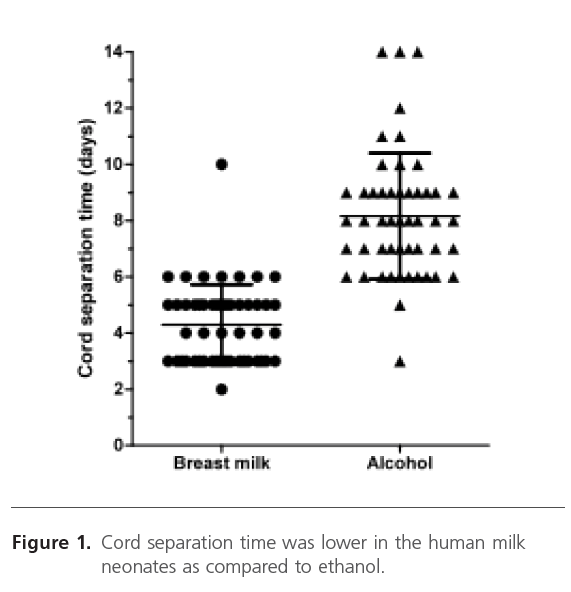
Figure 1: Cord separation time was lower in the human milk neonates as compared to ethanol.
Cord omphalitis signs and complications were less in the human milk neonates as compared to ethanol group neonates:
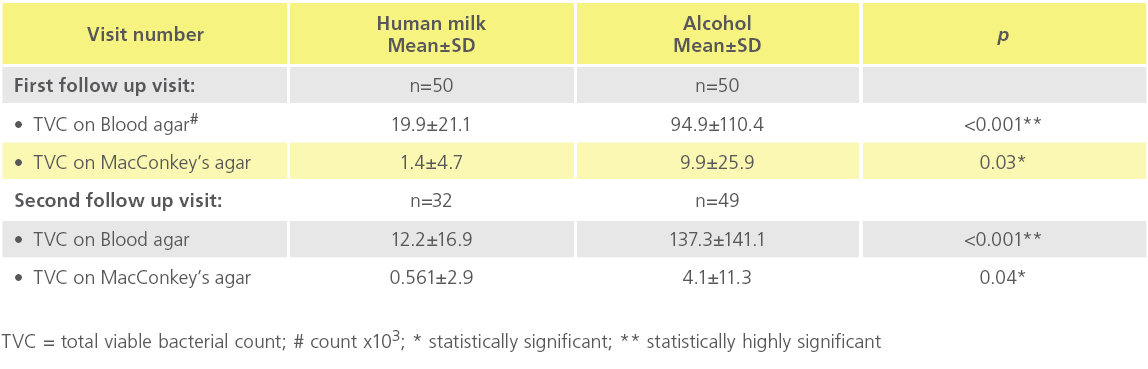
Table (3) shows that there were statistically significant differences (p<0.05) in all signs of omphalitis at the 3rd day visit (first visit) and the second visit (time of cord separation that varied among the study subjects as shown in Figure 1); such as skin color, presence of exudates, and hotness; between the human milk and alcohol groups. There was no significant difference in foul odor in both groups at the first visit, which was significantly different during the second visit. Body temperature was significantly lower in the human breast milk group during the first visit (p=0.001) but not in the second visit (p=0.07). There were no reported complications at the cord site in the human breast milk group while seven neonates (14%) did so in the ethanol group. In this regard, 2 (4%) of the subjects with complications had blood oozing and another 2 (4%) had cord remnants still present after separation. A deep gap wound at the cord site, hernia, and mucoid discharges were found at a frequency of one neonate (2%) each (data not shown in Table 3).
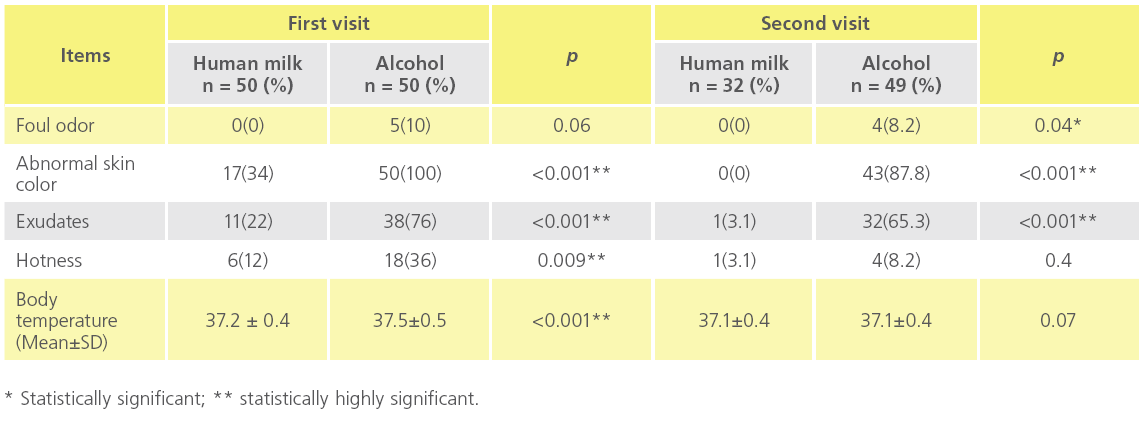
Table 3: Cord inflammation signs and complications were less in the human milk neonates as compared to ethanol group neonates during the first and second follow up visits.
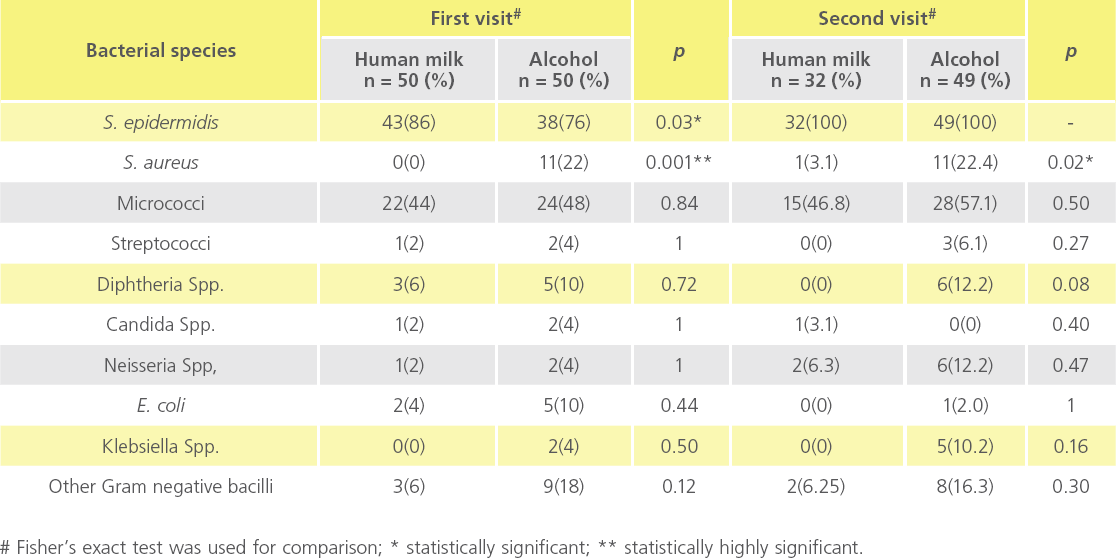
Human breast milk neonates had less colonization of the umbilical cord stump as compared to 70% ethanol treatment neonates:
Table (4) shows the TVC on blood and MacConkey’s agar. Neonates in the human milk group had statistically significant lower TVC when compared to the alcohol group neonates as determined on blood agar in the first and the second follow up visits (p<0.001 at both visits). TVC determined on MacConkey’s agar for babies treated with human milk was lower than alcohol group and differences were statistically significant at both the first (p=0.03) and second (p=0.04) follow up visits.
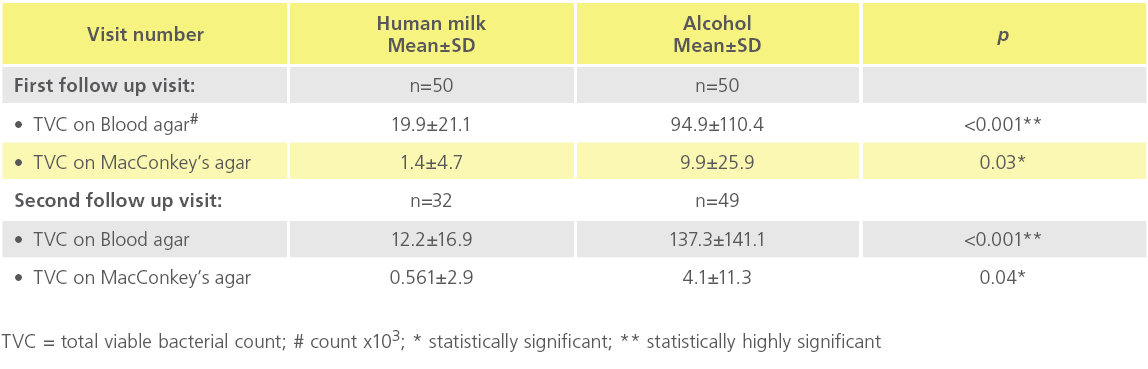
Table 4: Comparison between total viable bacterial count on blood and MacCkonkey’s agars among the human milk and alcohol groups during first and second follow up visits.
Human breast milk group neonates had less colonization of the umbilical cord stump with pathogenic organisms as compared to 70% ethanol treatment neonates at the first and the second follow up visits
Non pathogenic and pathogenic bacterial species on both blood and MacConkey’s agars in human milk- and alcoholcord care treatment groups are shown in Table 5. S. epidermidis populated cord stump of all neonates (100%) by the end of the second visit with a significant difference at the first visit. Importantly, S aureus, a pathogenic species; was significantly isolated at more frequency in the alcohol group neonates as compared to the breast milk neonates at both visits. Isolation of Micrococci, Streptococci, Diphtheria, Neisseria, Klebsiella species, E. coli, and other Gram negative bacilli was higher in the alcohol group neonates at both visits
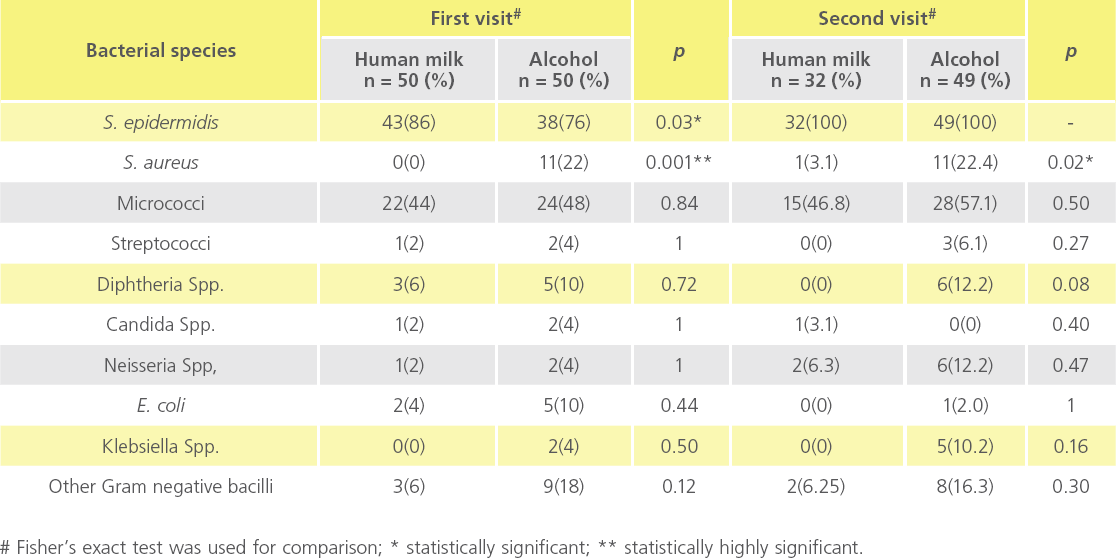
Table 5: Human breast milk neonates had less colonization of the umbilical cord stump with pathogenic organisms as compared to 70% ethanol treatment neonates at the first and the second follow up visits. Frequency of isolation in both visits is shown for both groups.
Discussion
In this study, we examined the effect of topical application of human breast milk on newborns’ cord separation time, omphalitis, and bacterial colonization and compared it to 70% ethanol in a quasi-experimental design at MUH. We found that the mean cord separation time in the human milk neonates was shorter (4.3±1.4 days) than that of alcohol (8.2±2.2 days). Cord omphalitis signs and complications were less in the human milk neonates as compared to ethanol group neonates. We also found a significant difference between the two groups in TVC of specimens collected from cord stump. The isolated organisms included S. epidermidis, S. aureus, Micrococci, E. coli and Klebsiella species, with higher rates of pathogenic species in the ethanol group. There are several reports of using breast milk for topical care of the umbilical cord [1,5,18] but they were compared with alcohol in only one study with a higher alcohol concentration 96% [5] and only one study and ours examined the effect of breast milk on colonization of the umbilical cord stump with different microorganisms. A similar observation was reported where the mean cord separation time in the human milk group was significantly shorter than 96% ethanol, an antiseptic silver sulfadiazine preparation [5] and dry cord care babies [18]. Another study [1], reported that the majority of the human milk-treated group (74%) had their cord fall off at the 6th- 10th day, which was longer than the duration reported in our study. The difference in cord separation time for human milk group could be attributed to differences in the number of the study subjects and/or the study settings.
Alcohol has been shown to delay cord separation when compared to other treatments [20]. Isopropanol has consistently been shown to lengthen cord separation time [21]. In addition, cases of acute alcohol toxicity in infants up to 21 days old have been reported after alcohol applications to the umbilical stump. Therefore, it is recommended that physicians and nurse practitioners should limit or avoid the use of alcohol for cord care [22-24]. In the current study, there were highly significant differences in cord omphalitis signs for both normal vaginal delivery (NVD) and cesarean section (CS) babies where the majority of babies had redness, exudates and elevated body temperature, while no statistically significant differences were found in all variables of cord inflammation signs.
Our data showed that the babies who had their umbilical cord cared with human milk had statistically significant decrease in the TVC as compared to ethanol group subjects during the first and the second follow up visits. This may be due to the anti-infective components present in the human milk. These data are in agreement with that of Paes & Jones [25], who reported that with alcohol cord care regimen, umbilical cord cultures showed a dramatic increase in bacterial colonization almost immediately after initiating alcohol cord care regimen. According to WHO, application of human milk to the cord stump is one of the cultural cord care practices used in Turkey, that could be beneficial in view of the antibacterial factors present in the breast milk [7]. Human milk has immunologic,anti-infective agents and colostrums containing significant quantities of complement components that act as natural antimicrobial agents. It, also, contains protective factors that provide specific and non specific passive immunity [18]. Human milk also contains IgA, which could contribute to the better action of human milk compared to ethanol. Colostrum, the milk produced by mothers in the first few days after birth, is especially rich in IgA [26]. Colostrum, also, contains higher amounts of white blood cells and infectionfighting substances than mature milk.
We found that there were statistically significant differences in colonization by S. epidermidis at the first follow up visit but not in the second follow up visit, where the cord stump of all neonates in both groups was populated by this organism (a normal skin flora). Our data showed that, when compared to alcohol group subjects, the cord stump of the human milk group neonates had lesser bacterial counts and reduced number of pathogenic microorganisms including S. aureus, E. coli and Gram negative bacilli with significant differences only in S. aureus. These data are supported by another report [18], that showed that colonization rate was statistically significant in the milk and alcohol groups with pathogenic microorganisms such as S. aureus, E. coli, K. pneumonia being lower in the human milk treatment group. However, they found that S. epidermidis was also higher in the breast milk group compared to dry cord care group [18]. In summary, this study showed that human milk treatment of the umbilical cord of the newborn babies compared to treatment with 70% ethanol was manifested by shorter cord separation time, lower inflammation signs and lower bacterial colonization; that were mainly of non pathogenic species.
Acknowledgment
We would like to thank Dr. Ashraf A. Ewis (Associate Prof. of Community Medicine and Public Health; Minia Faculty of Medicine) for his help with the statistical analysis of the data.
Funding
This study is supported by funds from Minia University and personal funds.
Competing interests and disclosures
All of the authors do not have any commercial or other association that might pose a conflict of interest.
2515
References
- Vural, G and Kisa, S (2006) Umbilical cord care: a pilot study comparing topical human milk, povidone-iodine, and dry care. J Obstet Gynecol Neonatal Nurs 35 (1), 123-128.
- Mullany, LC, Darmstadt, GL and Tielsch, JM (2003) Role of antimicrobial applications to the umbilical cord in neonates to prevent bacterial colonization and infection: a review of the evidence. Pediatr Infect Dis J 22 (11), 996-1002.
- Jellard, J (2002) Umbilical cord as reservoir of infection in a maternity hospital. Br Med J 1 (5024), 925-928.
- Sawardekar, KP (2004) Changing spectrum of neonatal omphalitis. Pediatr Infect Dis J 23 (1), 22-26.
- Ahmadpour-Kacho, M, Zahedpasha, Y, Hajian, K, Javadi, G and Talebian, H (2006) The effect of topical application of human milk, ethyl alcohol 96%, and silver sulfadiazine on umbilical cord separation time in newborn infants. Arch Iran Med 9 (1), 33-38.
- Barclay, L, Harrington, A, Conroy, R, Royal, R and Laforgia, J (2002) A comparative study of neonates’ umbilical cord management. Austr J Adv Nurs. 11, 34-40.
- WHO (2006) Postpartum care of mother and newborn, Care of the umblical cord.
- Magowan, M, Andrews, A, Pinder, B and Allen, S (1980) The effect of an antibiotic spray on umbilical cord separation times. Nurs Times 76 (42), 1841.
- Smales, O (1988) A comparison of umbilical cord treatment in the control of superficial infection. N Z Med J 101 (849), 453-455.
- Arad, I, Eyal, F and Fainmesser, P (1981) Umbilical care and cord separation. Arch Dis Child 56 (11), 887-888.
- Rais-Bahrami, K, Schulte, EB and Naqvi, M (1993) Postnatal timing of spontaneous umbilical cord separation. Am J Perinatol 10 (6), 453- 454.
- Verber, IG and Pagan, FS (1993) What cord care--if any? Arch Dis Child 68 (5 Spec No), 594-596.
- Ronchera-Oms, C, Hernandez, C and Jimemez, NV (1994) Antiseptic cord care reduces bacterial colonization but delays cord detachment. Arch Dis Child Fetal Neonatal Ed 71 (1), F70.
- Medves, JM and O’Brien, BA (1997) Cleaning solutions and bacterial colonization in promoting healing and early separation of the umbilical cord in healthy newborns. Can J Public Health 88 (6), 380-382.
- Dore, S, Buchan, D, Coulas, S, Hamber, L, Stewart, M et al. (1998) Alcohol versus natural drying for newborn cord care. J Obstet Gynecol Neonatal Nurs 27 (6), 621-627.
- Ford, LA and Ritchie, JA (1999) Maternal perceptions of newborn umbilical cord treatments and healing. J Obstet Gynecol Neonatal Nurs 28 (5), 501-506.
- WHO. (1998) Care of the Umbilical Cord: A review of the evidence, World Health Organization
- Farahani, L, Mohammadzaeh, A, Taffazzoli, M, Esmaeli, H and Ghazvini, K (2008) Effect of topical application of breast milk and dry cord care on bacterial colonization and umbilical cord separation time in neonates. Journal of Chinese Clinical Medicine 3 (6), 327-332.
- Nourian, M, Allaii, F and Heidari, A (2009) Comparison of the effect of alcohol 70% versus dry cord care on cord bacterial colonization and cord separation time among newborns. Pak J Med Sci 25 (1), 103-107.
- Mendenhall, A and Eichenfield, L (2000) Back to basics: Caring for the newborn´s skin. Contemp Pediatr 17, 98-114.
- Mullany, LC, Darmstadt, GL, Katz, J, Khatry, SK, LeClerq, SC et al. (2007) Risk factors for umbilical cord infection among newborns of southern Nepal. Am J Epidemiol 165 (2), 203-211.
- Darmstadt, GL and Dinulos, JG (2000) Neonatal skin care. Pediatr Clin North Am 47 (4), 757-782.
- Howard, R (2001) The appropriate use of topical antimicrobials and antiseptics in children. Pediatr Ann 30 (4), 219-224.
- Spray, A and Siegfried, E (2001) Dermatologic toxicology in children. Pediatr Ann 30 (4), 197-202.
- Paes, B and Jones, CC (1987) An audit of the effect of two cord-care regimens on bacterial colonization in newborn infants. QRB Qual Rev Bull 13 (3), 109-113.
- Kelly, D and Coutts, AG (2000) Early nutrition and the development of immune function in the neonate. Proc Nutr Soc 59 (2), 177-185.