Perspective - (2024) Volume 14, Issue 4
Toxicology of Analgesics: Understanding the Risks and Management
Dharminder Chauhan*
Department of Toxicology, University of Pharmagen, Maharastra, India
*Correspondence:
Dharminder Chauhan, Department of Toxicology, University of Pharmagen, Maharastra,
India,
Email:
Received: 02-Jul-2024, Manuscript No. IPFT-24-14971;
Editor assigned: 05-Jul-2024, Pre QC No. IPFT-24-14971 (PQ);
Reviewed: 19-Jul-2024, QC No. IPFT-24-14971;
Revised: 01-Aug-2024, Manuscript No. IPFT-24-14971 (R);
Published:
29-Aug-2024
Introduction
Analgesics, commonly known as painkillers are medications
used to relieve pain. They are widely available Over-The-Counter
(OTC) or via prescription and are generally considered safe when
used as directed. However, like all medications, analgesics come
with risks, especially when misused or taken in excess.
Understanding the toxicology of analgesics is crucial for
healthcare professionals and the general public to ensure safe
and effective use.
Description
Mechanisms of action
Analgesics work through various mechanisms to reduce pain
perception. They can broadly be classified into non-opioid (such
as NSAIDs and acetaminophen) and opioid analgesics. Nonopioid
analgesics like NSAIDs inhibit cyclooxygenase enzymes,
thereby reducing prostaglandin synthesis and inflammation.
Acetaminophen, though its exact mechanism is not fully
understood, is thought to act centrally on pain pathways.
Opioid analgesics, on the other hand, exert their effects by
binding to opioid receptors in the central nervous system,
modulating pain perception. These receptors are also
responsible for the addictive potential of opioids, making them a
subject of significant clinical concern.
Types of analgesics and their mechanisms
Analgesics can be categorized into several classes based on
their mechanisms of action and chemical structure:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs
such as ibuprofen, naproxen and aspirin work by inhibiting the
enzyme Cyclooxygenase (COX), thereby reducing inflammation
and pain.
Acetaminophen: Also known as paracetamol, acetaminophen
works centrally in the brain to reduce pain perception and fever.
Unlike NSAIDs, it has minimal anti-inflammatory effects.
Opioids: Opioids like morphine, oxycodone and codeine exert
their analgesic effects by binding to opioid receptors in the
central nervous system, blocking pain signals.
Each class of analgesic has its own toxicity profile, which varies
based on factors such as dose, duration of use and individual
susceptibility.
Toxicological risks of analgesics
Despite their benefits, analgesics can cause adverse effects
and toxicity, particularly when used improperly:
NSAIDs: Prolonged use of NSAIDs can lead to gastrointestinal
complications such as ulcers, bleeding and perforation. Renal
toxicity is also a concern, especially in patients with pre-existing
kidney disease.
Acetaminophen: While generally safe at recommended doses,
acetaminophen overdose can cause severe liver damage. This is
a significant concern because acetaminophen is a common
ingredient in many OTC medications and can be inadvertently
overdosed.
Opioids: The main risk associated with opioids is respiratory
depression, which can be fatal in overdose situations. Opioid
toxicity is a growing public health concern due to the risk of
addiction and overdose deaths.
Management of analgesic toxicity
Prompt recognition and management of analgesic toxicity are
essential to prevent serious complications:
NSAIDs: Treatment of NSAID toxicity involves discontinuing
the medication and supportive care. Severe cases may require
gastrointestinal protection or in rare instances, surgical
intervention.
Acetaminophen: Early administration of N-Acetylcysteine
(NAC) is crucial in acetaminophen overdose to prevent liver
damage. NAC replenishes depleted glutathione stores, reducing
the toxicity of acetaminophen metabolites.
Opioids: Opioid toxicity is managed with naloxone, an opioid
antagonist that reverses respiratory depression and other opioid
effects. Timely administration of naloxone can save lives in cases
of opioid overdose.
Prevention strategies
Preventing analgesic toxicity begins with education and
awareness:
Patient education: Healthcare providers should educate
patients about proper analgesic use, including dosage
instructions, potential side effects and the importance of not
exceeding recommended doses.
Monitoring: Regular monitoring of patients using analgesics,
especially long-term NSAIDs or opioids, can help detect toxicity
early.
Combination products: Patients should be cautious with
combination products containing multiple analgesics (e.g.,
acetaminophen and opioids) to avoid unintentional overdose.
Regulatory considerations
Regulatory agencies play a critical role in ensuring the safety
of analgesics:
Labeling and Warnings: Regulatory bodies mandate clear
labeling of analgesic medications, including dosing instructions,
warnings about potential risks and information on safe use.
Opioid prescribing practices: In response to the opioid
epidemic, regulatory measures have been implemented to
restrict opioid prescribing practices, enhance prescriber
education and improve access to opioid reversal agents like
naloxone.
Challenges in clinical practice
Despite advancements in toxicology and medical
management, several challenges persist in the clinical use of
analgesics:
Patient education: Many cases of analgesic toxicity stem from
inadvertent misuse or lack of understanding of dosage
instructions. Educating patients about the risks and proper use of
analgesics is crucial.
Polypharmacy: The simultaneous use of multiple analgesics
or medications increases the risk of adverse drug interactions
and toxicity. Careful consideration of drug combinations and
patient-specific factors is essential.
Over-the-counter availability: Easy accessibility of analgesics
without prescription increases the likelihood of self-medication
and overdose, particularly with acetaminophen.
Conclusion
Understanding the toxicology of analgesics is vital for
healthcare professionals and the public to mitigate risks
associated with these commonly used medications. While
analgesics provide effective pain relief when used appropriately,
misuse or overdose can lead to serious health consequences. By
promoting safe prescribing practices, educating patients and
implementing regulatory measures, we can enhance the safe
use of analgesics and reduce the incidence of analgesic toxicity
in the population. Vigilance, education and timely intervention
are key to ensuring the safe and effective use of analgesic
medications in clinical practice.
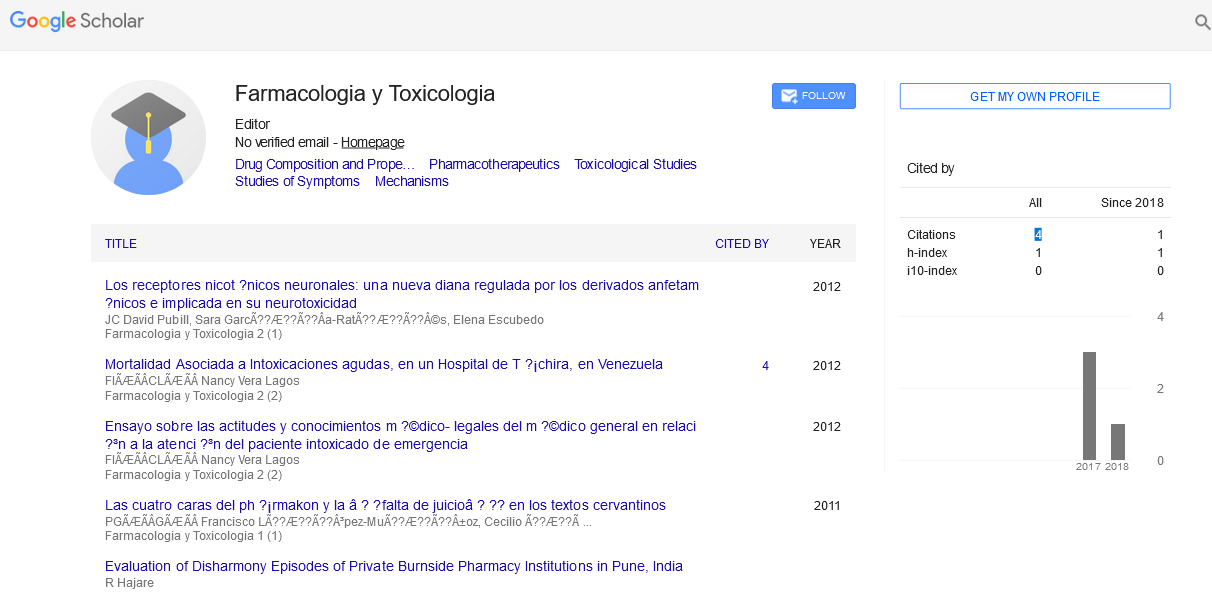
Citation: Chauhan D (2024) Toxicology of Analgesics: Understanding the Risks and Management. Farmacologia Toxicologia, Vol.14 No.4: 034