Keywords
Hyphema; Blunt trauma; Intraocular pressure; Visual acuity; Cataract; Glaucoma
Introduction
Hyphema refers to the presence of blood within the anterior chamber of the eye; Traumatic hyphema was fairly common following blunt trauma and result from damage to an iris or angle vessel [1].
Eye injuries still remain one of the most common causes of unilateral blindness worldwide. Blunt eye injuries mostly result in traumatic hyphema and are not an infrequent cause of presentation to the emergency unit of many eye clinics. Most result from unnecessary eye injuries, which are largely preventable [2-8].
Hyphema is one of the most challenging clinical problems encountered by the ophthalmologist. Traumatic hyphema is encountered in children and adults. Hyphema is usually the result of a projectile or deliberate punch that hits the exposed portion of the eye despite the protection of the bony orbital rim. Various missiles and objects have been incriminated, including balls, rocks, projectile toys, air guns pellets and the human fist [9,10].
There have even been cases involving objects larger than the orbit, Such as soccer balls [11].
With the increase of child abuse, fists and belts have started to play a prominent role. Males are involved in three fourths of cases [12].
Because changes in the eye following trauma can result in significant elevations of IOP, it is presumed that optic nerve damage will occur if the pressure remains high enough long enough. Although glaucomatous optic neuropathy may take some time to develop, elevated IOP after ocular trauma can occur immediately after the injury or at any time in the future, even years later [13].
All over the world, the mean annual incidence of hyphema is approximately 17 patients in 100,000 with a peak incidence between 10 and 20 years [14].
In urban areas, two thirds of traumatic hyphema is due to blunt ocular trauma [15].
Review of Literature
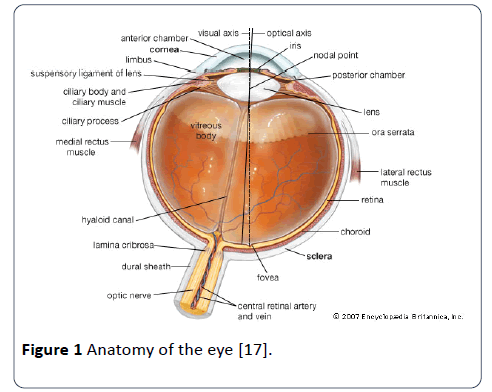
The anatomy of the human eye
Cornea: The transparent part of the eyeball which covers the iris and pupil.
Sclera: The white, dense, fibrous outer coating of the eyeball.
Iris: The coloured diaphragm in the anterior chamber of the eyeball which contracts and expands to adjust for light intensity.
Pupil: The opening in the centre of the iris through which light passes.
Lens: The transparent, dual-convex body which focuses light rays onto the retina.
Retina: The membrane on the inner wall of the eyeball which receives the image from the lens and converts it into nerve impulses.
Vitreous gel: A clear jelly-like substance which fills the posterior chamber of the eyeball, normally attached to the retina.
Optic nerve: Transmits nerve impulses from the retinal cell layers to the brain [16].
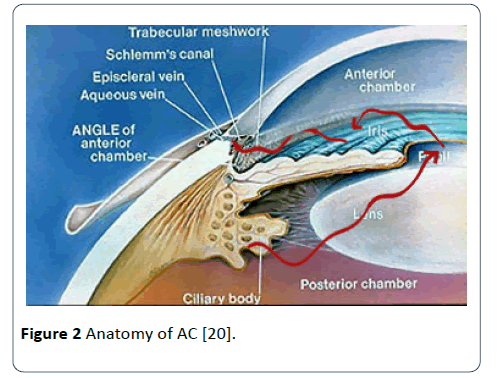
Anterior chamber: Is bound in front by the cornea and posteriorly by the anterior iris surface and the pupillary portion of the lens. The lateral recess of the anterior chamber is formed by the iridocorneal angle occupied by the trabecular meshwork. The anterior chamber is deepest centrally (3 mm) and shallowest at the peripheral insertion of the iris, and contains approximately 250 ml of aqueous humour. The aqueous humour is drained from the anterior chamber chiefly via the trabecular (conventional) pathway into Schlemm’s canal then into the collector channels the episcleral veins to the superior vena cava [17-19] (Figures 1 and 2).
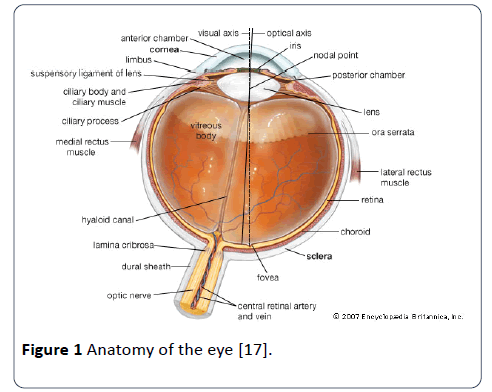
Figure 1: Anatomy of the eye [17].
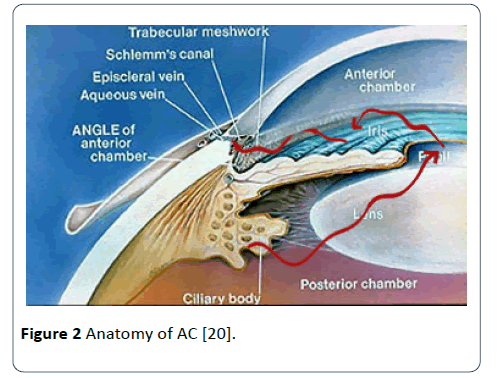
Figure 2: Anatomy of AC [20].
Blunt ocular trauma
The term blunt ocular trauma describes a condition in which the eye is subjected to a trauma by an object that does not penetrate the eye and is one of the most important causes of ocular morbidity in childhood [20,21].
Various missiles and objects have been incriminated, including balls, rocks, projectile toys, air gun pellets and the human fist [22].
Other causes of blunt trauma are tennis and squash balls, elastic luggage straps and champagne corks. Most ocular trauma in children occurs during casual play with other children. Older children and adolescents are most likely to be injuries while participating in sports. Children 11-15 years old have a particularly high incidence of severe eye injury compared with other age groups. Injured boys outnumber girls by a factor of 3 or 4 to 1 [21].
Blunt ocular trauma can cause both structural and functional damage to the eye [23].
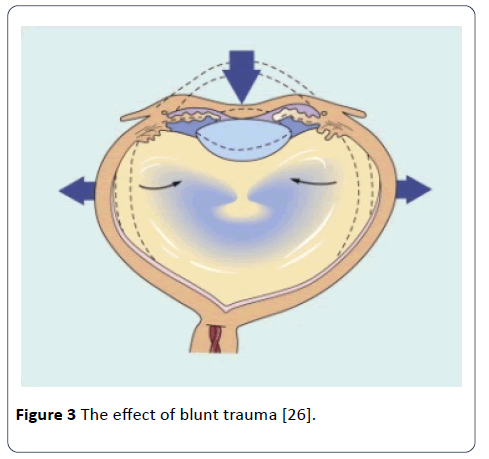
It produces a shockwave that is transmitted posteriorly through the eye [24].
Severe blunt trauma causes a compression of the anteroposterior diameter of the globe and a simultaneous expansion at the equatorial plane [25].
With a transient but severe increase in intraocular pressure, although the impact is primarily absorbed by the iris-lens diaphragm and the vitreous base, damage can also occur at a distant site such as the posterior pole. The extent of ocular damage depends on the severity of trauma. Apart from obvious ocular damage, blunt ocular trauma may result in long term effects so that the prognosis is necessarily guarded (Figure 3).
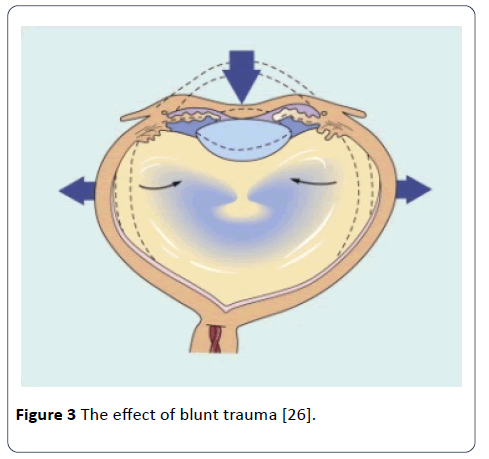
Figure 3:The effect of blunt trauma [26].
The following complications can happen (corneal erosion, corneal abrasion, acute corneal oedema, tears in descemet’s membrane, hyphema, pupil miosis, iris pigment imprinting on the anterior lens capsule called vossius ring, traumatic mydriasis, radial tears in pupillary margin, iridodialysis, traumatic aniridia, ciliary body shock resulting in hypotony, angle recession, traumatic uveitis, cataracts, lens subluxation, lens dislocation, globe rupture, PVD, vitreous haemorrhage, commotion retinae, choroidal rupture, retinal breaks, retinal detachment, optic neuropathy and optic nerve avulsion) [22].
Epidemiology of blunt traumatic hyphema
Incidence: The annual incidence of traumatic hyphema has been estimated at 17 injuries per 100,000 populations, with males being affected three to five times more frequently than females [25-27].
Up to 70 percent of traumatic hyphema occurs in children, with a peak incidence between 10 and 20 years of age [2,26,27].
Ocular trauma has a huge economical coast due to hospitalization and medical bills and lost working hours [15].
Pathogenesis of blunt traumatic hyphema
Blunt ocular trauma, producing indentation of the anterior surface of the eye, causes stretching of Limbal tissue, equatorial scleral expansion, posterior and peripheral movement of the aqueous humour, posterior displacement of lens or iris diaphragm, and acute elevation of IOP. This can cause tearing of tissue near the anterior chamber angle. Most hyphema (71-94%) result from tears in the anterior face of the ciliary body, with disruption of the major arterial circle and its branches, recurrent choroidal arteries, or ciliary body veins, the remaining percentage arises from ruptured iris vessels, cyclodialysis, or iridodialysis [25,28].
The importance and significance of hyphema lies in the fact that when hyphema is severe it is associated with a significant rise in the intraocular pressure (IOP) that may cause damage to the optic nerve if severe and prolonged and this will lead to permanent deterioration of vision. Also hyphema may be associated with other serious complications that affect vision corneal blood staining [29] and damage to other vital eye structure. Hyphema is also more severe and associated with more complications in those with sickle cell haemoglubinopathies which is also more difficult to treat because the biochemical and metabolic conditions in the aqueous humour favour erythrocyte sickling, and as a result, sickle erythrocytes can plug the outflow pathways and cause increased intraocular pressure even with small hyphema [30].
Types of blunt traumatic hyphema
Primary: This is fairly innocuous and transient.
Secondary: Usually more severe (rebleed) and occur several days to 2 weeks following the original bleed (most commonly within the first 5 days). This probably occurs due to normal thrombolysis of the original clot prior to repair of the damaged blood vessel, and can totally fill the anterior chamber (eight ball hyphema after the black pool ball) [1,31].
Grading of blunt traumatic hyphema
Depending on the risk of rebleeding, hyphema can be divided into two grades:
1. Grade 1, Low risk (small hyphema occupying less than half of the anterior chamber, Caucasian) [32].
2. Grade 1, High risk (large hyphema occupying more than half of the anterior chamber, Afro-Caribbean, raised IOP, secondary bleed) [32].
Clinical features of blunt traumatic hyphema
Symptoms:
1. Blurred vision by the hyphema itself or damage to other intraocular structures. This may be worse on walking as the hyphema can settle across the pupil while the patient is sleeping.
2. Dull ache in and around the eye if there is an associated rise in the intraocular pressure.
3. Diplopia if there is an associated orbital fracture [1,22].
Signs:
1. Red blood cells circulating within the aqueous humour in the anterior chamber termed microhyphema.
2. Red blood cells settle (sediment) inferiorly with a resultant ‘fluid’ level, the height of which should be measured and documented.
3. With time, all becomes settled and starts to contract as it dissipated; it may even separate with a whitish surface layer.
4. Signs of other intraocular damage (corneal oedema, iris damage, angle recession, zonular dehiscence leading to lens phakodonesis or subluxation or dislocation, retinal dialysis, retinal detachment, vitreous detachment, choroidal rupture, commotion retinae, etc. [1,22].
Investigations of blunt traumatic hyphema
1. Blood test (patient of Afro-Caribbean ancestries who experience a hyphema re-investigated with a blood smear to look for sickle cell haemoglubinopathies.
2. Ultrasonography of the eyeball, when there is no fundus view, to exclude posterior segment damage [1,22].
Hyphema related IOP elevation and glaucoma
The IOP fluctuation after an injury of the globe is as follows:
1. A moderate elevation (up to 24 mmHg) immediately after the injury with a duration of 6-18 hours, due to mechanical obstruction of the trabecular meshwork from blood constituents and inflammatory debris. In addition, there can be a direct injury and a following oedema of the trabecular meshwork.
2. Recovery of the IOP in normal values or even hypotony. The latter is observed from the 2nd until the 4th or 5th day and increases significantly the risk of a secondary haemorrhage. The cause of the hypotony is the reduction of the aqueous humour production due to ciliary body trauma.
3. Gradual increase of the IOP beginning the 5th-6th day that can reach high values. The reason for this phenomenon is dual: the return of the ciliary body function and the sustained obstruction of the aqueous humour circulation.
4. A return of the IOP in normal values due to the absorption of the blood and the reinstitution of the trabecular meshwork function after approximately 4-18 days [33-36].
Inflammatory cells and other particulate debris (e.g., blood, fibrin, and iris pigment and lens material) can mechanically block the outflow pathways, which may lead to pupillary block and secondary angle closure, or open-angle glaucoma due to outflow pathway obstruction [13].
Ghost cell glaucoma with hyphema may cause elevated intraocular pressure 2 weeks to 3 months after the initial injury. Gradual clearing of the hyphema occurs, with erythrocytes losing haemoglobin and becoming so-called ghost cells, with resultant trabecular blockage due to the distorted, bulky configuration of the crenate red blood cell [37].
Finally, patients should be observed closely with Gonioscopy when the eye is stable, because approximately 20% to 94% of those who develop hyphema experience associated anglerecession glaucoma especially when the recession is 180° and more [36].
Management of blunt traumatic hyphema
The management of blunt traumatic hyphema is usually conservative:
Grade 1, Low risk (small hyphema less than half of the anterior chamber, Caucasian):
1. Outpatient bed rest (except in children and active patient who must be admitted in hospital).
2. Dilation (controversial) with long acting Mydriatics like atropine or homatropine twice or 3 times/day to check for posterior segment damage and to prevent further bleeding and to treat associated traumatic uveitis and pain and to keep the iris dilated to prevent excessive iris movement, as this may predispose to a rebleed.
3. Patients should be reviewed in several days to check the intraocular pressure.
4. Any pressure rise is treated on its merits with topical antiglaucomatous medication, oral acetazolamide or even hyperosmotic a agent such as mannitol.
5. Topical steroids to treat the traumatic uveitis and to reduce the risk of secondary haemorrhage.
6. Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDS) should be avoided because of their antithrombotic effect.
7. The patient should be advised to present immediately if they have symptoms of a rebleed with decreased vision or ocular ache.
8. Patients should also be advised to avoid vigorous physical activity for several weeks following a hyphema as this may predispose to a rebleed [1,22,31,32].
Grade 2, High risk (large hyphema more than half of the anterior chamber, Afro-Caribbean, raised IOP, Secondary bleed):
1. In-patient bed rest.
2. Dilation (controversial).
3. Patient reviewed daily until the hyphema has substantially resolved.
4. Treat associated rise in IOP.
5. Topical Steroids.
6. No NSAIDS.
7. Oral antifibrinolytic e.g. tranexamic acid (Cyclokapron) 15-25 mg/kg/ b.d or/ t.i.d can reduce the risk of rebleeding.
8. Some clinicians use systemic or (more recently) topical aminocaproic acid 50 mg/kg/q.i.d, an antifibrinolytic agent, to stabilize the clot and thereby reduce the risk of a secondary haemorrhage. This is usually used only with a complete hyphema (‘eight-ball’ hyphema) or where there has already been one rebleed.
9. Surgical evacuation (washing) of the blood in the anterior chamber with or without Trabeculectomy is indicated in the following circumstances:
A – IOP> 50 mmHg for 2 days or > 35 mmHg for 7 days.
B – Early corneal blood staining because it can progress to a dense opacity within a few hours.
C – Total hyphema for more than 5 days to prevent the development of PAS and chronic elevation of IOP [1,22,30,32].
Objectives
The following objectives were set for the study:
Frequency of problem, most common causes and ocular health insult.
1. To evaluate the unaided visual acuity and intraocular pressure level on discharge of blunt traumatic hyphema management.
2. To compare between Grade 1 (low risk) hyphema and grade 2 (high risk) hyphema regarding the final visual outcome on discharge.
Material and Methods
The overall design
The study was a retrospective (descriptive) survey of all blunt traumatic hyphema patients admitted in Shaheed Dr. Aso Teaching Eye Hospital in Sulaimani City, Kurdistan Region of Iraq during the period from January 1, 2008 to December 31, 2008.
Data collection
Every patient attending or referred to the emergency department suffering from a blunt trauma to the eye and has hyphema on examination is usually admitted in the hospital and has a registration file containing serial number, demographic, medical information, ophthalmic information, examination notes and management during every day stay in the hospital.
In the registration file a full history was taken from each patient including the senior doctor in charge for the patient, age of the patient, gender, occupation , date of admission, date of discharge, affected eye and cause of blunt trauma.
The patients were divided into two groups (according to their risk to develop a secondary bleeding), group 1 (grade one) of low risk (hyphema filling less than half of the anterior chamber) and group 2 (grade two) of high risk (hyphema filling more than half of the anterior chamber or hyphema associated with high intraocular pressure) to compare between them regarding the final visual outcome.
All the details regarding the associated damage to other structures of the eye by the blunt trauma were reviewed thoroughly and patients were divided into four groups (those with no damage, those with anterior segment damage, those with anterior and posterior segment damage and those with ruptured globe).
The initial unaided visual acuity and the initial level of intraocular pressure on admission were recorded for comparisons with the same parameters on discharge in order to assess the final outcome of the management on discharge.
For statistical analysis regarding the objectives of this study, all the everyday treatment along with examination notes of the senior doctor (UVA, IOP, slit-lamp examination) of each patient were recorded in order to have a clear idea about the progress of the condition.
Statistical analysis
The different variables chosen as demographic information of each patient and treatment modalities for hyphema management are analyzed for frequencies using the (Epi Info) program which is public domain statistical software for epidemiology developed by centres of Disease Control and Prevention (CDC) in Atlanta, Georgia (USA).
Other results were analyzed using statistical package for social science (SPSS) software (version 13). Categorical variables were tested using the person’s Chi Square test and P value of less than 0.05 was considered significant.
Results
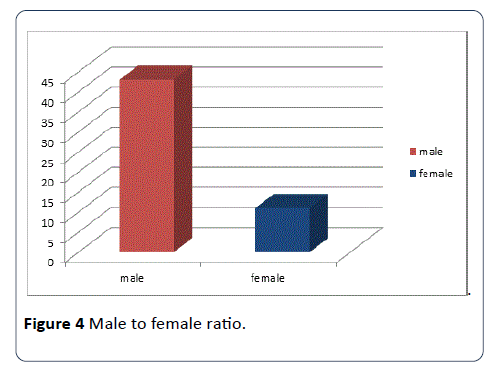
The registration files of 54 patients (those who were admitted to Shaheed Dr. Aso Eye Hospital suffering from Blunt traumatic hyphema) were studied thoroughly and out of these 54 patients, 43 (79.6%) were males and 11 (20.4%) were females. A male to female ratio was 3.9:1 (Figure 4).
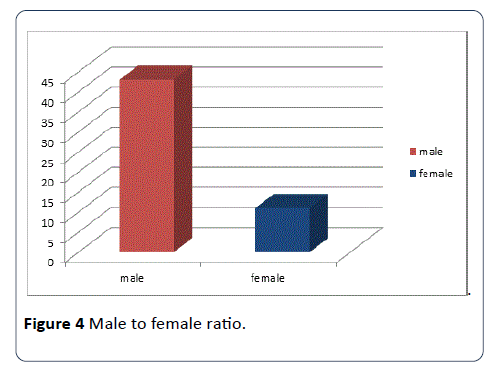
Figure 4: Male to female ratio.
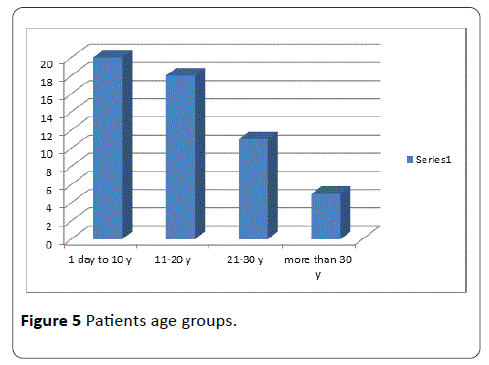
The age of the patients ranged from 3 to 57 years (mean age was 16.34 years). The presenting complaint in most of the patients was reduction in vision due to a blunt traumatic hyphema. Thirty one patients (57.4%) had the blunt traumatic hyphema in their left eye and twenty three patients (42.6) in their right eye. Left eye to right eye ratio was 1.35:1 (Figure 5).
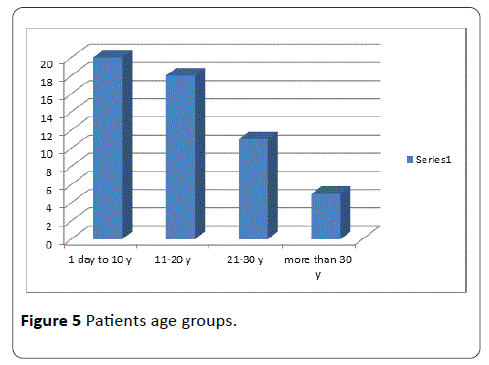
Figure 5: Patients age groups.
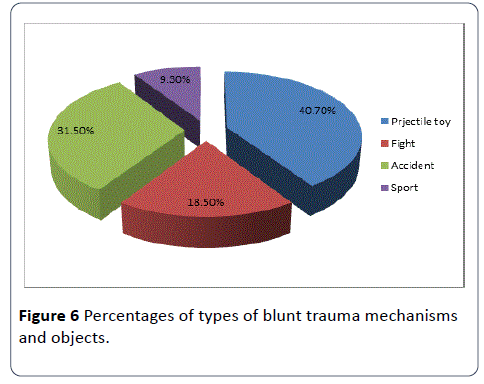
The cause of the blunt trauma was a projectile toy in 22 patients (40.7%), an accident in 17 patients (31.5%), a hit during fights in 10 patients (18.5%) and a sport related trauma in 5 patients (9.3%) (Figure 6).
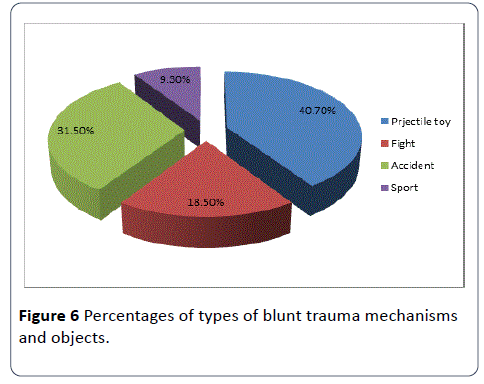
Figure 6: Percentages of types of blunt trauma mechanisms and objects.
Patients’ duration of hospitalization ranged from 1 to 13 days (mean was 2.9 days). Twenty nine patients (53.7%) had their blunt traumatic hyphema during holidays, while twenty five patients (46.3%) during the other days. Number of holidays was 74 days during the year 2008.
Regarding the occupation of the patients, twenty nine patients (53.7%) were students; nine patients (16.7%) were preschool children, nine patients (16.7%) had free jobs, 4 patients (7.4%) had no jobs and 3 patients (5.6%) were employee.
Regarding the type of hyphema, all the patients (54 patients, 100%) were presented with a primary bleeding, fifty patients (92.6%) had only a primary bleeding and only four patients (7.4%) had a secondary rebleed during their admission in the hospital.
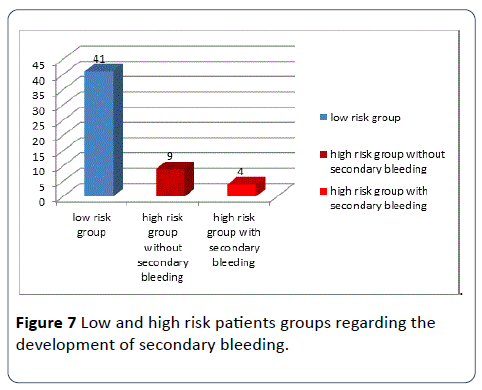
The patients were divided into 2 groups (according to their risk to develop a secondary bleeding), group 1 (grade 1, low risk, 41 patients, 75.9%) and group 2 (grade 2, high risk, 13 patients, 24.1%) (Figure 7).
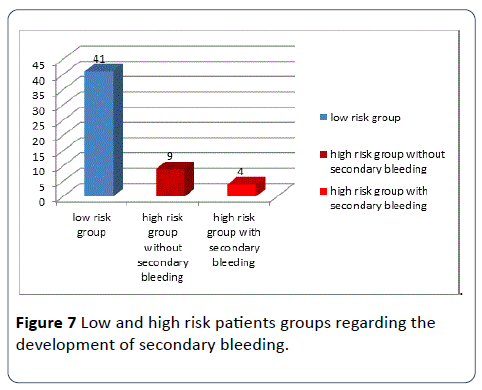
Figure 7: Low and high risk patients groups regarding the development of secondary bleeding.
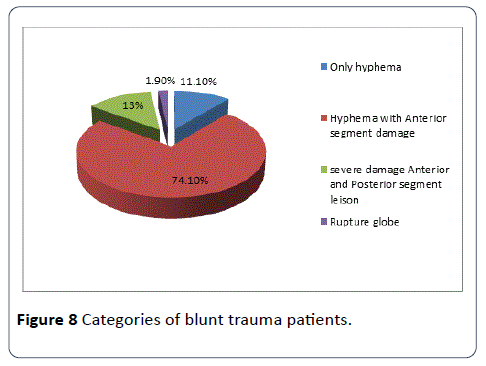
Forty patients (74.1%) had damages to the anterior segment of the eyeball with the hyphema on presentation, seven patients (13%) had damages to the anterior and posterior segment of the eyeball with the hyphema, Six patients (11.1%) had no associated damages (only hyphema), while only one patient (1.9) presented with a ruptured globe with the hyphema (Figure 8).
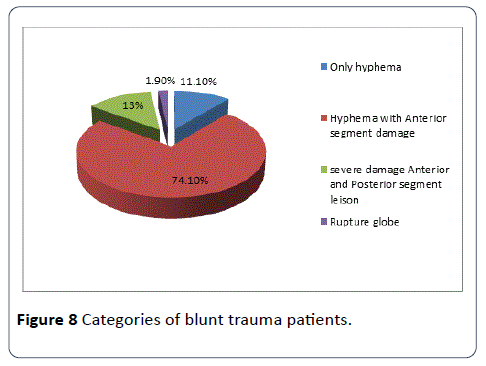
Figure 8: Categories of blunt trauma patients.
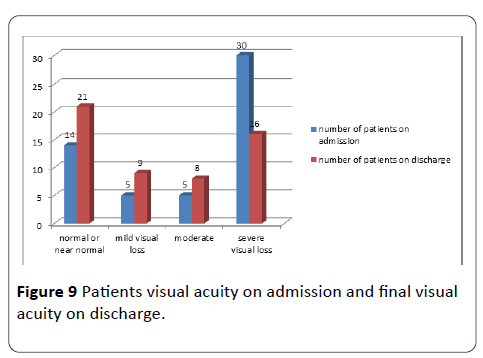
Unaided visual acuity of the patients on admission ranged from 6/6 to no light perception (examined using the illiterate E chart), 14 patients (25.9%) had a normal or near normal UVA (6/6-6/9), 5 patients (9.3%) had a mild reduction in the UVA (6/12-6/18), 5 patients (9.3%) had a moderate reduction in the UVA (6/24-6/36), and 30 patients (55.6%) had a severe reduction in the UVA (6/60 and worse). On discharge, 21 patients (38.9%) had a normal or near normal UVA (6/6-6/9), 9 patients (16.7%) had a mild reduction in the UVA (6/12-6/18), 8 patients (14.8%) had a moderate reduction in the UVA (6/24-6/36), and 16 patients (29.6%) had a severe reduction in the UVA (6/60 and worse) (Figure 9).
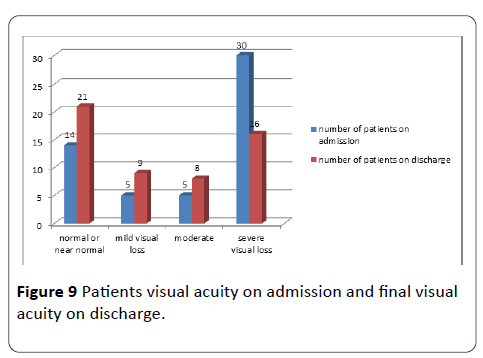
Figure 9: Patients visual acuity on admission and final visual acuity on discharge.
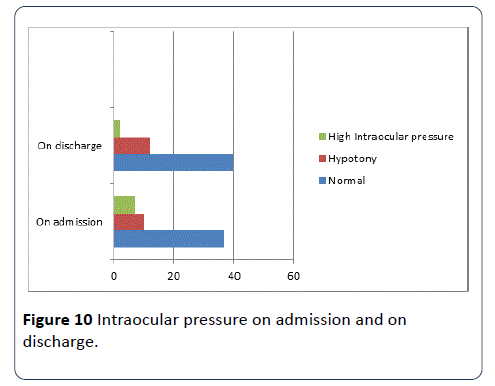
The level of intraocular pressure of the patients on admission ranged from zero to 30 mmHg (mean was 15.37 mmHg), thirty seven patients (68.5%) had a normal IOP (11-21 mmHg), ten patients (18.5%) had hypotony (IOP <11 mmHg) mainly due to a concomitant ciliary body shutdown, and seven patients (13%) had an elevated IOP >21 mmHg mainly due to a large hyphema >½ AC.
On discharge, the number of patients with normal IOP increased to 40 (74.1) and the number of patients with hypotony also increased to 12 (22.2%) while the number of patients with elevated IOP reduced to 2 (3.7%), mainly due to the use of antiglaucoma medication and absorption of the hyphema (Figures 8 and 10).
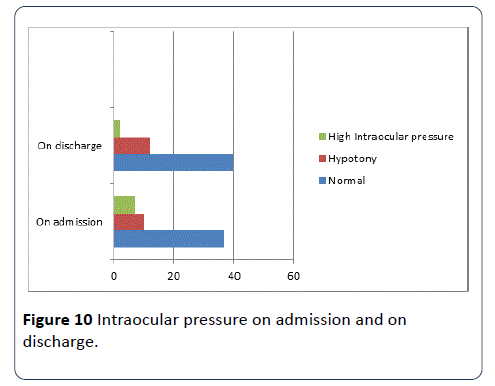
Figure 10: Intraocular pressure on admission and on discharge.
Regarding the instruction that were given to the patients, 32 patients (59.3%) were instructed to have a complete bed rest while 22 patients (40.7%) were not, three patients (5.6%) were instructed to have their head elevated when lying on bed wile 51 patients (94.4%) were not, five patients (9.3%) were instructed to restrict their physical activity while 49 patients (90.7%) were not, and four patients (7.4%) were observed frequently while 50 patients (92.6%) were not.
Regarding medical treatment, 47 patients (87%) were given antibiotics (whether systemic or local) while 7 patients (13%) were not, 51 patients (94.4%) were given steroids (whether systemic or local) while 3 patients (5.6%) were not, 29 patients (53.7%) were given Cycloplegics (local) while 25 patients (46.3) were not, 13 patients (24.1%) were given antiglaucoma medication (whether systemic or local) while 41 patients (75.9%) were not, and 33 patients (61.1%) were given a systemic antifibrinolytic medication (tranexamic acid, Cyclokapron) while 21 patients (38.9%) were not.
No surgical intervention (anterior chamber paracentesis) was done for the patients due to the fact that there was no indication for it according to the criteria that we followed in this study, only one patient (with the ruptured globe) had an operation to close the rupture.
The result showed that the UVA of the patients on discharge had no significant association with the different types of medical treatment and the severity of associated eyeball damage.
Discussion
In the results, blunt traumatic hyphema was more common in males than in females; this is similar to the reports from Western Europe, America< Asia and Africa 2-8 and 43.
This is because males all over the world are more indulged in playing activities, sports and fights than females.
The results showed that blunt traumatic hyphema was more common among children and young adolescent students <20 years of age, and the left eye was more commonly involved than the right. These finding were observed in several previous studies [38,39].
This may be a reflection of the fact that children and young adolescent participates in playing activities and fights more than adults and elderly, and there are more right-handed people, also missiles or sticks used with the right hand are more likely to affect the left eye [35].
The results also showed that the most common cause of blunt traumatic hyphema was a projectile toy (40.7%) but this is not the case in the other studies around the world like Papaconstantinou D et al. [14].
WHO reported that assault was the most common cause (45.8%); this is because of the difference in cultures and environments. The low occurrence of sports injuries in our population suggest the low priority given to sports, and this may be due to poor information about its benefits. In recent studies from developed countries, Sports related injuries have become the most common in adults [40-42].
With enforcement of appropriate legislation, work-related eye injuries have been reduced. However, increasing prosperity that makes more time available for sports and increased awareness of the health benefits of sports have increased sports injuries, up to 68% in some studies [42,43].
Also in the results we noticed an increase in the number of hyphema during holidays (including festival days and national holidays, 53.7%), the same with the results of Bouhaimed Manal et al. [44], this is because of the large number of projectile toys sold to children during these days and the extra time of leisure.
Secondary bleeding occurred only in 4 patients (7.4%) during their stay in the hospital, but other reports give a wide range from 0.4% to 38% mainly due to the difference in the risk factors for developing a secondary bleed [45-47].
In the results, those with grade 2 hyphema were 24.1% which is less than that found in Pakistan and Nigeria [8], 43 who reported about 50% of the patients to have a grade 2 hyphema, but different from that reported by Edward and Layden [2]. In the latter study, only 15% of patients had grade 2 hyphema. This is all due to the fact that such types of trauma in our society are less than those in other parts of Asia and Africa but still high compared to the developed world in America and Europe.
The final visual outcome on discharge in patients who presented with blunt traumatic hyphema was relatively good (better than 6/60) in 70.4% of our patients but poor (6/60 or worse) in 29.6%, a third of patients in the present work, compared to 96% in those reported by Shiucy and Lucarelli [48,49] and 75% of those reported by Kearn [50], achieved visual acuity of 6/18 or better. This visual outcome is worse than in other patients in North America [43], Europe [15,49] but is similar to report from Asia and other parts of Africa [8,43]. This may have been due to several factors in our setting like the grade of hyphema, poor UVA on admission due to severe eyeball damage (ruptured globe, retinal detachment and previous trauma) and due to non-compliance of the patients with the doctor’s instruction.
Also Grade 1 hyphema had a better final visual outcome on discharge than Grade 2 hyphema just like the results reported by Kearns [49,50], mostly due to the large size of the bleeding or raised IOP that have more harmful effect on vision than small or uncomplicated hyphema.
The significant association between the grade of hyphema and the UVA on discharge in the result was also observed by Cho [50], who reported that the large hyphema were associated with the worse visual outcome due to their more prolonged harmful effects. Also the finding that there was no significant association between the different types of medical treatments and the UVA on discharge in those patients was also noticed by Rocha et al. [51], who reported that the treatment was controversial and does not lead to improvement in those with low visual acuity on admission. While there was no significant association between the other eyeball structure damage and the UVA on discharge in the results, Sheppard JD [52] reported that the presence of other eyeball structure damage is a poor prognostic factor for the visual acuity on discharge especially if the posterior segment of the eyeball is involved, this is because of the difficulty in assessing the severity of hyphema associated other eyeball structure damage and because of the short duration of hyphema patient’s admission in our hospitals.
Finally, the assumption that the all patients had a pretrauma 6/6 vision was a source of bias in the results because of the fact that refractive errors and other causes were responsible for the reduced vision on admission other than the blunt traumatic hyphema itself.
Conclusions
From the results, we can conclude the following:
1. Hyphema is a self-limiting complication of blunt trauma and most commonly of grade 1, so the management if conservative to prevent a secondary bleeding.
2. Most of our hyphema patients were males and <20 years as they indulge more than others in playing activities (most commonly by projectile toys) and fights especially during holidays and festival days without adult supervision.
3. One third of our patients had a poor unaided visual acuity on discharge mostly due to grade 2 hyphema and severe associated eyeball damage.
4. The prognosis of the final outcome (the UVA and IOP level) on discharge of blunt traumatic hyphema management depends on the grade of hyphema, proper patient instruction and proper management to prevent a secondary bleeding.
5. Grade 1 (low risk) hyphema had a better visual outcome on discharge than grade 2 (high risk) hyphema.
Recommendations
1. As the level of hyphema inside the anterior chamber of the eye is important as an indicator of developing a secondary bleeding that has a major impact on the visual acuity of the eye, a careful examination by the ophthalmologist is mandatory for guiding the best suited management of each patient based on the grade of hyphema, and to keep in mind that secondary bleeding could happen up to 2 weeks after the primary one, so frequent observation is the rule.
2. Refraction of the best corrected visual acuity and careful Gonioscopy to detect angle recession for all hyphema patients prior to discharge should be the rule.
3. Careful and close supervision by adults over all types of projectile toys played by children, especially during festivals and holidays.
4. Emphasizing on wearing eye protecting goggles during sports to reduce the incidence of blunt traumas to the eyes, and trying to make wearing these goggles mandatory for all players. Also to forbidden all types of projectile toys that do not meet the safety regulations legislated by the government, and encouraging the population no to buy them for sake of their children safety.
5. To do stronger studies on the long term management and follow up of blunt traumatic hyphema patients (especially those of grade 2 and posterior segment damage) because of the possibility of long term complications of the eye.
6. All of the victims of blunt trauma should be encouraged to have their eyes checked for any possible complications that might endanger their vision and to comply fully with all the regulations given by their doctors.
7. To improve quality of life for persons who are partially sighted from the effect of hyphema, by providing facilitated emergency departments, ophthalmology specialists, low vision specialists, social workers and support groups.
8. Making a strong cooperation between internists and ophthalmologists for early detection and referral of blunt traumatic hyphema.
9. Finally, the importance of patient education, health care team education and affordable eye care should be emphasized by ophthalmologists, to reduce cases of visual impairment due to blunt traumatic hyphema.
18306
References
- Bruce AS, Loughnan MS (2003) Anterior eye disease and therapeutics A – Z (1st edn.). Elsevier, Netherlands. pp: 164-165.
- Edwards WC, Layden WE (1973) Traumatic hyphema: A report of 184 consecutive cases. Am J Ophthalmol 75:110-116.
- Agapitos PJ, Leon-Paul N, Clarke WN (1987) Traumatic hyphema in children. Ophthalmology 94:1238-1241.
- Luksza L, Homziuk M, Nowakowska-Klimek M, Glasner L, Iwaszkiewicz-Bilikiewicz B (2005) Traumatic hyphema caused by eye injuries. KlinOczna 107:250-251.
- McEwen CJ, Baires PS, Desai P (1999) Eye injuries in children: the current picture. Br J Ophthalmol 83:933-936.
- Spoor TC, Kwitko GM, O’Grady JM, Ramocki JMI (1990) Traumatic hyphema in an urban population. Am J Ophthalmol 109:23-27
- Amoni SS (1981) Traumatic hyphema in Kaduna, Nigeria. Brit J Ophthalmol 65:439-444.
- Morris DS (2006) Ocular blunt trauma: Loss of sight from an ice hockey injury. Br J Sports Med 40:e5.
- Listman DA (2004) Paintball injuries in children: more than meets the eye. Pediatrics 113:e15-18.
- Kent JS, Eidsness RB, Colleaux KM, Romanchuk KG (2007) Indoor soccer-related eye injuries: should eye protection be mandatory? Can J Ophthalmol 42:605-608.
- Crouch ER, Frenkel M (1976)Aminocaproic acid in the treatment of traumatic Hyphema.Am J Ophthalmol 81:355-360.
- Choplin NT(2003)Glaucoma associated with ocular trauma. In:Choplin NT (ed.)Ophthalmic care of the Combat Casualty.Army MedicalCenter,Washington.pp: 185-194
- Papaconstantinou D, Georgalas I, Kourtis N, Karmiris E, Koutsandrea C, et al. (2009) Contemporary aspects in the prognosis of traumatic Hyphema.ClinOphthalmol3: 287-290.
- Walton W, Hagen VS, Grigorian R, Zarbin M (2002) Management of traumatic hyphema. SurvOphthalmol 47:297-334.
- Read JE, Goldberg MF (1974) Traumatic hyphema: Comparison of medical treatment. Trans Am AcadOphthalmolOtolaryngol 78:799.
- Snell, Richard S (2004) Clinical anatomy (7th edn.). Lippincott Williams and Wilkins. pp: 832-833.
- Leisegang TJ, Skuta GL, Cantor LB(2003) Basic and Clinical Science Course: Section 6 Paediatric Ophthalmology and Strabismus. American Academy of Ophthalmology, San Francisco, CA.
- Kaushik S, Sukhija J, Pandav SS, Gupta A (2006) Blunt ocular trauma in one eye. Ann Ophthalmol 38: 249-252.
- Kanski, Jack J (2007) Clinical ophthalmology: A systemic approach (6th edn). Butterworth- Heinemann, UK. pp: 854-855.
- Spalton DJ, Hitching RA, Hunter PA, James CHT, Harry J(2006) Atlas of clinical ophthalmology.
- Kanski, Lack J (2007)Retinal detachment. Clinical ophthalmology: A systemic approach(6th edn). Butterworth-Heinemann, UK. p. 708.
- Kennedy RH, Brubaker RF (1988) Traumatic hyphema in a defined population. Am J Ophthalmol 106:123.
- Thomas J,Gang L, Skuka GL, Cantor LB(2003-2004) Basic and Clinical Science Course:Section 13International Ophthalmology. Chapter XI, Ocular Trauma Epidemiology and prevention.American Academy of Ophthalmology, San Francisco, CA.
- Berrios, Ramon R, Dreyer, Evan B (1995) Traumatic hyphema. IntOphthalmolClin: Winter 35: 93-103.
- Noble BA, Simmons IG, Chang BYP(2002) Anterior segment repair and reconstruction (Techniques and Medico – Legal issue). The damaged pediatric eye. Butterworth-Heinemann, UK. p. 112.
- Noble BA, Simmons IG, Chang BYP(2002) Anterior segment repair and reconstruction (Techniques and Medico – Legal issue). Primary response- the principles of management of surgical complications and the repair of ocular injuries.Butterworth-Heinemann, UK. pp:15-16.
- Layden WE (1974) Traumatic glaucoma. Trans Am AcadOphthalmolOtolaryngol 78:346-351.
- Ashaye AO (2008) Traumatic hyphema: A report of 472 consecutive cases. BMC Ophthalmol 8:24.
- Sihota R, Kumar S, Gupta V, Dada T, Kashyap S, et al. (2008) Early predictors of traumatic glaucoma after closed globe injury: trabecular pigmentation, widened angle recess, and higher baseline intraocular pressure. Arch Ophthalmol 126:291-296.
- Campbell DG (1981) Ghost cell glaucoma following trauma. Ophthalmology 8:1151-1158.
- Jan S, Khan S, Mohammad S (2003) Hyphema due to blunt trauma. J Coll Physician Surg Pak 13:398-401.
- Yospaiboon Y, Sangveejit J, Suwanwatana C (1989) Traumatic hyphema: Clinical study of 149 cases. J Med Assoc Thai 72:520-526.
- Bouhaimed M, Alwohaib M, Alabdulrazzaq S, Jasem M (2009) Toy gun ocular injuries associated with festive holidays in Kuwait.Graefes Arch ClinExpOphthalmol 247: 463-467.
- Mela EK, Dvorak GJ, Mantzouranis GA, Giakoumis AP, Blatsios G, et al. (2005) Ocular trauma in a Greek population: Review of 899 cases resulting in hospitalization. Ophthalmic Epidemiology 12:185-190.
- Calzada JI, Kerr NC (2002) Traumatic hyphema in children secondary to corporal punishment with a belt. Am J Ophthalmol 135:719-720.
- Lai JC, Fekrat S, Barrun Y, Goldberg MF (2001) Traumatic hyphema in children: Risk factors for complications. Arch Ophthalmol 119:64-70.
- McEwen CJ (1989) Eye injuries: A prospective survey of 5671 eyes. Br J Ophthalmol 73:888-894.
- Witteman GJ, Brubaker SJ, Johnson M, Marks RG (1985) The incidence of rebleeding in traumatic hyphema. Ann Ophthalmol 17: 528-529.
- Thomas MA, Parrish RK, Feuer WJ (1986)Rebleeding after traumatic Hyphema. Arch Ophthalmol 104:206-210.
- Rahmani B, Jahadi HR, Rajaeefard A (1999) An analysis of risk for secondary hemorrhage in traumatic hyphema. Ophthalmology 106:380-385.
- Shiucy Y, Lucarelli MJ (1998) Traumatic hyphema: outcome of outpatients’ management. Ophthalmology 105:851-855.
- Kearns P (1991) Traumatic hyphema: A retrospective study of 314 cases. Br J Ophthalmol75:137-141.
- Baker RS, Wilson MR, Flowers CW, Lee DA, Wheeler NC (1996) Demographic factors in a population – based survey of hospitalized, work – related ocular injury. Am J Ophthalmol 122:213-219.
- Rocha KM, EngelI DP, GusmãoI FBA, MartinsII EN, Moraes NSB(2004) Traumatic hyphema: One year follow-up.Arq BrasOftamol 67: 133-137.