Image Article - (2022) Volume 14, Issue 10
Tuberculous psoas abscess
Kondanath Saifudheen1* and
Ariwala Muhammad Ali2
1Consultant Neurologist, Department of Neurology, Jeddah National Hospital, Jeddah, P.O Box 8564, Jeddah 21492, Saudi Arabia
2Consultant Radiologist, Department of Radiology, Jeddah National Hospital Jeddah, Saudi Arabia
*Correspondence:
Kondanath Saifudheen, Consultant Neurologist, Department of Neurology, Jeddah National Hospital, Jeddah, P.O Box 8564, Jeddah 21492,
Saudi Arabia,
Tel: 966535172966,
Email:
Received: 25-Oct-2022, Manuscript No. ipaom-22-13132;
Editor assigned: 25-Oct-2022, Pre QC No. P-13132;
Reviewed: 26-Oct-2022, QC No. Q-13132;
Revised: 27-Oct-2022, Manuscript No. R-13132;
Published:
04-Nov-2022
Clinical-Medical Image
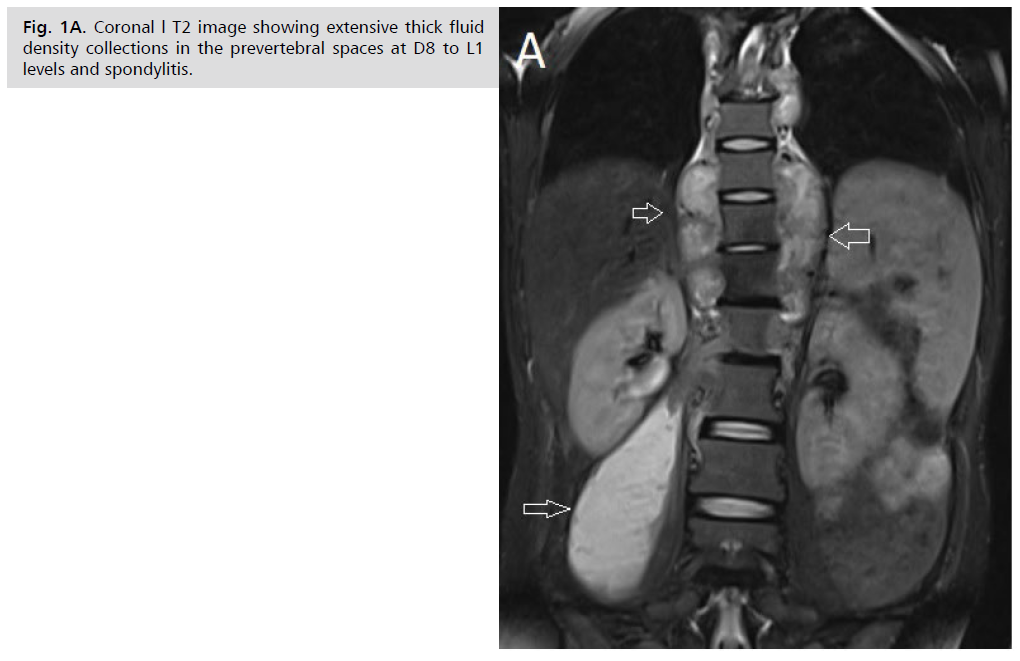
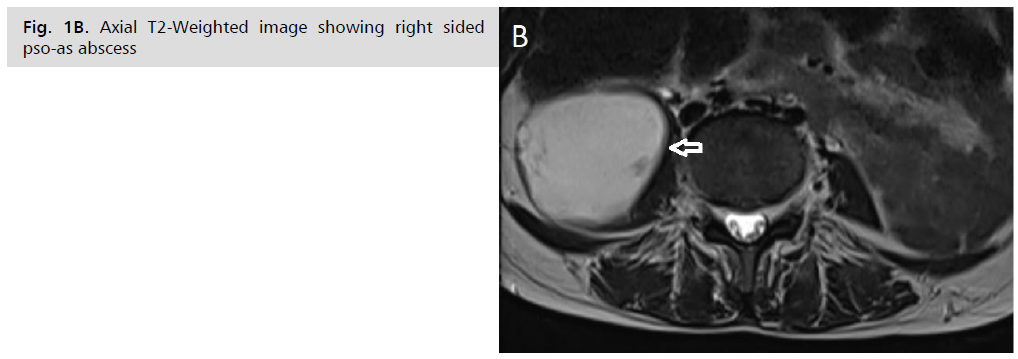
A 35-year-old lady who was originally from Ethiopia presented to our clinic with 1-month history of progressive back pain, fever, anorexia. The physical examination was remarkable for tenderness dorsal spine and a temperature of 38°C. Serologic HIV testing was negative. Blood test showed an increased C-reactive protein (40 mg/ dl), without any others abnormalities. Chest radiograph showed no abnormal infiltration or opacity . Magnetic resonance imaging coronal T2 revealed extensive thick fluid density collections in the prevertebral spaces at D8 to L1 levels and spondylitis. (Figure 1 A, white arrows), On right side the fluid extends into the right psoas muscle resulting large psoas abscesses. (Figure 1 B, whiten arrows). CT-guided aspiration of the right psoas yielded 300 ml of pus and the results of Ziehl–Neelsen staining of collection were positive, and culture showed Mycobacterium tuberculosis indicating Pott’s disease with Psoas abscess. Mycobacterium tuberculosis grew in a culture of the tissue, indicating Pott’s disease. Antituberculous chemotherapy was prescribed. Subsequent radiographic studies showed that psoas abscesses had regressed, and the patient’s clinical symptoms improved within 3 months
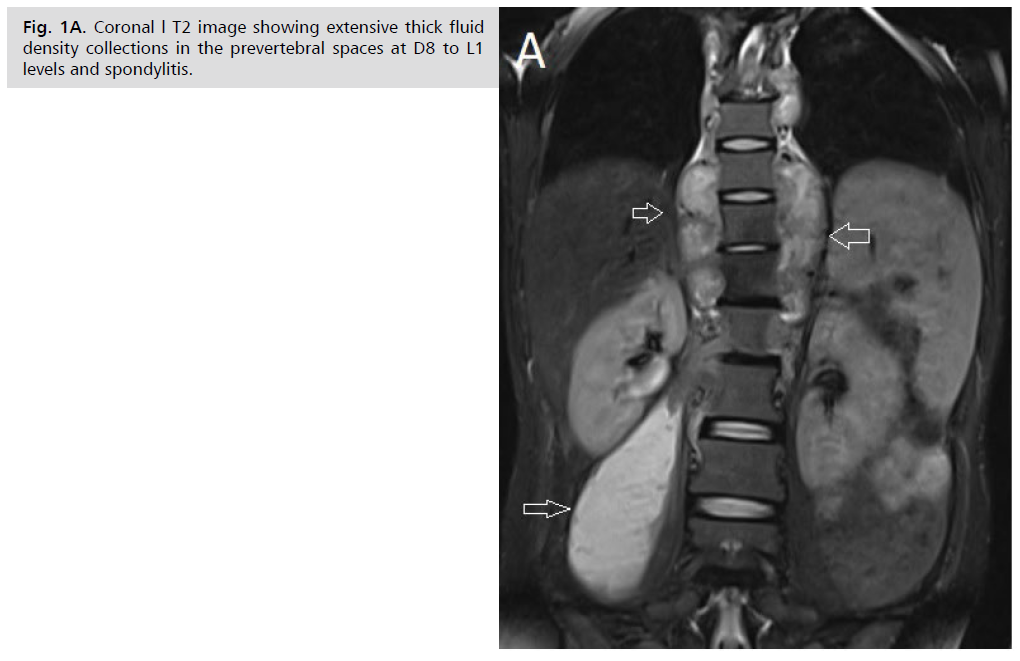
Figure 1A: Coronal l T2 image showing extensive thick fluid density collections in the prevertebral spaces at D8 to L1 levels and spondylitis.
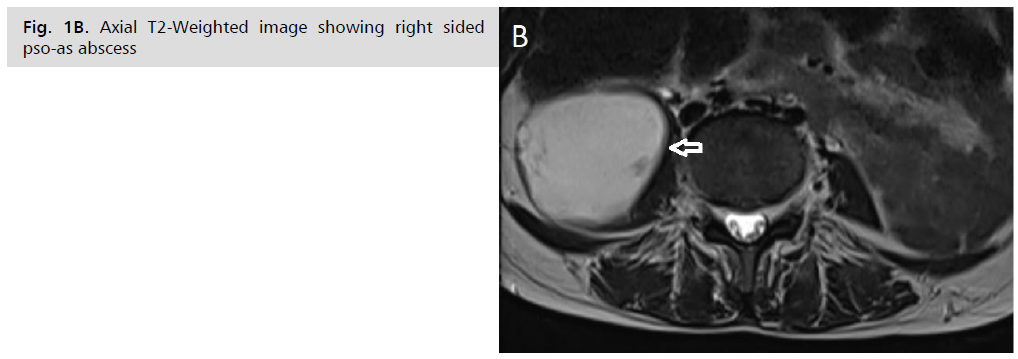
Figure 1B: Axial T2-Weighted image showing right sided pso-as abscess
Psoas muscle abscess is a relatively rare condition that is difficult to diagnose because of the non-specific clinical presentation. It may be primary or secondary to intra-retroperitoneal or osteo-articular infection. The most frequently found germs are Staphylococcus aureus in primary abscesses and Escherichia coli [1] in secondary abscesses. Tuberculous origin is rare, especially in developed countries but is still relevant in endemic countries.
Osteoarticular tuberculosis represents 3–5 % of cases of tuberculosis and 15 % of cases of extrapulmonary tuberculosis. It affects all segments, but lumbar spine involvement remains most common [2].
The clinical picture is insidious and nonspecific, which leads to delayed diagnosis and treatment. Although fever, abdominal or back pain and limitation of hip joint movements are the classical triad of psoas abscess, it can be presented only in 35% of all patients [3].
Clinical suspicion, radiological study either with Ultrasound, CT or MRI, along with microbiological culture of the pus, are crucial to the diagnosis. The treatment consists of percutaneous or surgical drainage combined with antituberculous treatment for a minimum of 9-12 months.
REFERENCES
- Miloudi, Mouhcine, Soufiane Belabbes, Mohammed Sbaai et al. Psoas abscess due to Candida tropicalis: a case report. Ann Biol Clin. 2018;76 (5):571-573.
Google Scholar, Crossref, Indexed at
- Rafiqi, K., B. Yousri, M. Arihi, C. Bjitro et al. Unusual locations of osteoarticular tuberculosis in children: a report of 12 cases. Orthop Traumatol Surg Res. 2013;99 (3): 347-351.
Google Scholar, Crossref, Indexed at
- Penado, Susana, Belén Espina and Juan Francisco Campo. Absceso de psoas. Descripción de una serie de 23 casos. Enferm Infecc Microbiol Clin. 2001;19(6): 257-260.
Google Scholar, Crossref, Indexed at