Keywords
Unilateral Eales; Case report Eales; Steroids; Jarisch–Herxheimer reaction; Anti-Tuberculous drug in Eales disease; Combined steroids and antituberculous in eales; Steroid monotherapy in eales; Anti-tuberculous monotherapy in eales; Eales disease with presumed tubercular etiology
Introduction
Henry Eales, in 1880, reported this illness as an abnormal retinal vein, neovascularization in the periphery, and recurrent vitreous hemorrhage associated with constipation and epistaxis, as noninflammatory condition [1,2]. But later Elliot has described as retinal vasculitis [3] with the tendency of Asian origin [1]. It is a primary occlusive peripheral retinal vasculitis and considered as an idiopathic entity [4], but recently, it is postulated to be multifactorial. The disease is characterized by peripheral retinal phlebitis then progresses to the venous sheathing, then occlusion phase starts, which causes ischemia and neovascularization, giving rise to the hallmark of the disease to occur, which are recurrent vitreous and retinal hemorrhages [4]. This illness affects healthy males in their second to third decades, as a peak age of onset [5] but can range from 13-63 years in reported cases, and up to 90% of the men have bilateral disease [4].
The exact etiology of Eales' disease is still controversial, but it had been postulated to be multifactorial [2], and the most strongly associated etiologies were both hypersensitivity to tuberculoprotein and tuberculosis [6]. A considerable number of the Mycobacterium tuberculosis DNA and the polymerase chain reaction (PCR), had been recovered from the vitreous samples of the Eales' patients [4,5,7-9]. Also, the Mycobacterium tuberculosis genome had been demonstrated in the epiretinal membrane samples of the Eales patients when compared to the controlled group, which tested for nested PCR; statistically, a significant correlation has been shown [10]. The human leukocyte antigen (HLA) also play roles in the etiology of this illness like HLA DR1, DR4, B5 [4,7]. The presence of nested PCR in the epiretinal membrane can have an impact on the HLA predisposition to develop retinal vasculitis secondary to cell-mediated response triggered by sequestered Mycobacterium tuberculosis [10].
Here, we present three cases of unilateral Eales disease with presumed tubercular etiology presented with different gender, age, presentation and treatment.
Case Presentation
Case number 1
A 52 years old man presented to our clinic with a sudden onset of the floaters in the left (OS) eye over a few days. A review of systems was normal for all medical and surgical issues with no history of using any drug.
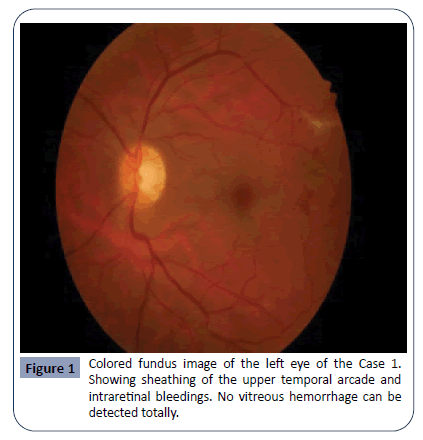
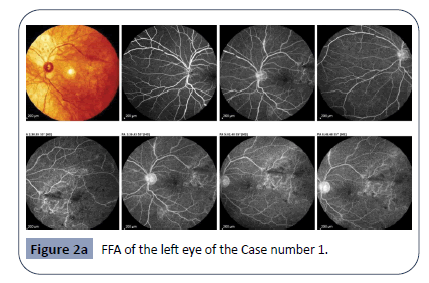
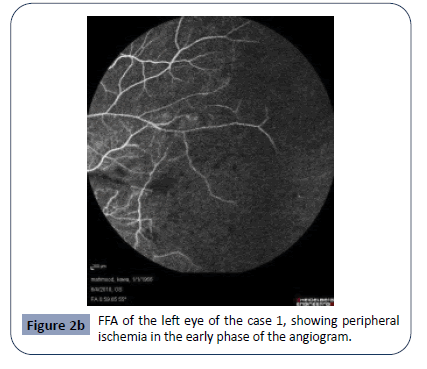
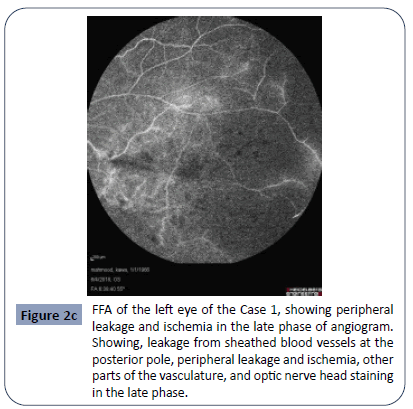
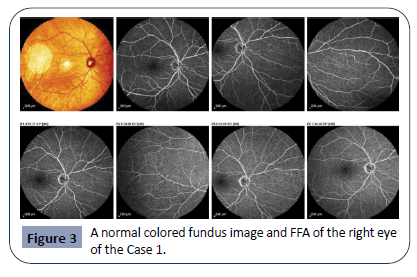
Ophthalmological examinations reviewed his best-corrected visual acuity (BCVA) was 6/6 for both eyes (OU). The anterior segment (AS) and intraocular pressure (IOP) were normal. The dilated fundus examination revealed minimal and slight vitreous hemorrhage, vitreous cells, healthy optic nerve, perivascular sheathing in the distal part of the upper arcade, dotted intraretinal hemorrhages, non-perfused areas from the temporal macula to the temporal periphery. No neovascularization detected, Figure 1. Fundus fluorescein angiography (FFA) of the left eye showed leakage from the sheathed vessel, vascular tortuosity, clear cut demarcation of capillaries in the non-perfused area, the venous shunt showed as a demarcation line between perfused and nonperfused area, telangiectasia in the temporal part of the macula, and staining of the optic nerve head in the late phase of the angiogram, Figure 2a Figure 2b and Figure 2c. Right eye FFA is entirely normal. The hyperfluorescent ring appearing around the optic nerve head is a normal finding and indicates staining of the bare sclera around the optic nerve head. Only (QuantiFERONTB Gold) and tuberculin skin test were positive, while other investigations were negative, Table 1.
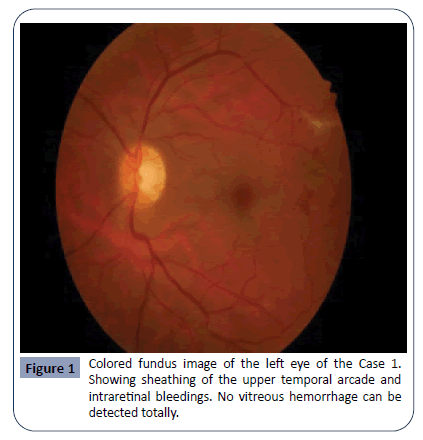
Figure 1: Colored fundus image of the left eye of the Case 1. Showing sheathing of the upper temporal arcade and intraretinal bleedings. No vitreous hemorrhage can be detected totally.
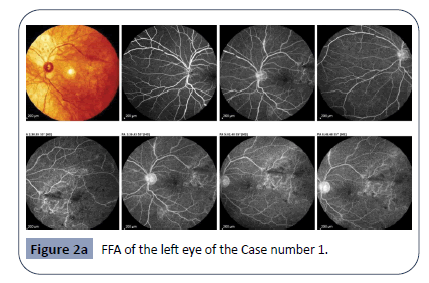
Figure 2a: FFA of the left eye of the Case number 1.
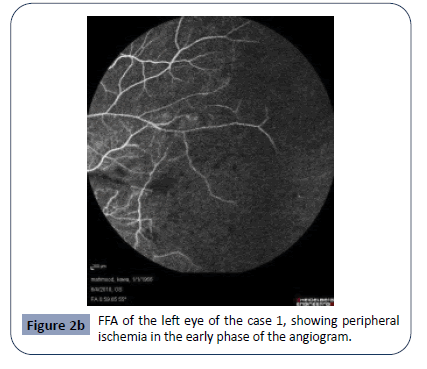
Figure 2b: FFA of the left eye of the case 1, showing peripheral ischemia in the early phase of the angiogram.
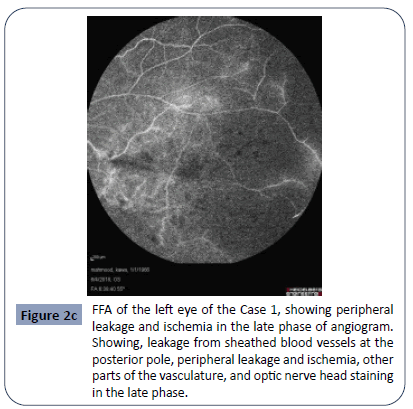
Figure 2c: FFA of the left eye of the Case 1, showing peripheral leakage and ischemia in the late phase of angiogram. Showing, leakage from sheathed blood vessels at the posterior pole, peripheral leakage and ischemia, other parts of the vasculature, and optic nerve head staining in the late phase.
Table 1: Different tests for all cases.
| |
Case 1 |
Case 2 |
Case 3 |
| CBP, ESR and Hb electrophoresis |
Normal |
Normal |
Normal |
| CRP |
Normal |
Normal |
Normal |
| ANA |
Normal |
Normal |
Normal |
| HIV |
Normal |
Normal |
Normal |
| VDRL |
Non-reactive |
Non-reactive |
Non-reactive |
| (QuantiFERON-TB Gold) |
Positive |
Positive |
Positive |
| PPD |
Positive (19mm) |
Positive (17 mm) |
Positive (19 mm) |
| Chest X-ray |
Normal |
Normal |
Normal |
Regarding lines of treatment
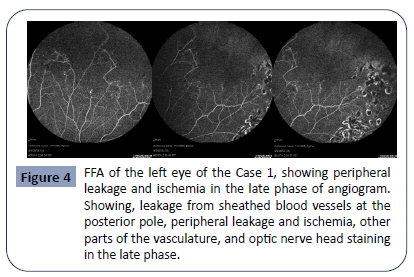
The ischemic area treated with argon laser and the patient first received only prednisolone 1mg/kg/day (5), and on the subsequent checkup the patient was completely asymptomatic and but peripheral fundus showed new intraretinal hemorrhages, the new FFA showed the new ischemic area in continuation with the old one and treated with argon laser Figure 4. Then the patient treated with full anti-tuberculous therapy for one year covered with oral steroids for three months to suppress inflammatory reaction and to prevent Jarisch–Herxheimer's reaction to happen. After completing one-year treatment, no new ischemic area has occurred on FFA, and the visual acuity did not change all over the course (Figures 1-4).
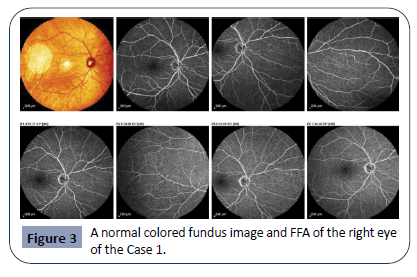
Figure 3: A normal colored fundus image and FFA of the right eye of the Case 1.
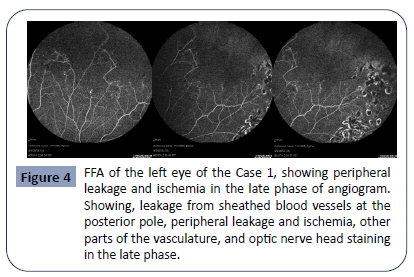
Figure 4: FFA of the left eye of the Case 1, showing peripheral leakage and ischemia in the late phase of angiogram. Showing, leakage from sheathed blood vessels at the posterior pole, peripheral leakage and ischemia, other parts of the vasculature, and optic nerve head staining in the late phase.
Case number 2
A 55 years old male nurse, not known to have any systemic illness, presented with sudden onset of floaters in the right (OD) eye, after she had been treated with prophylactic laser photocoagulation for peripheral retinal hole ten days earlier, elsewhere.
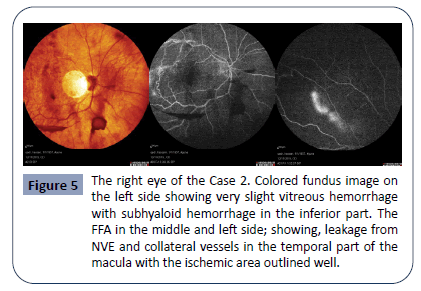
On ocular examination, her VA was 6/18 OD, uncorrected with glasses and the OS 6/6. The AS and IOP were normal OU, and the posterior segment examination showed mild vitreous and subhyaloid hemorrhage with the peripheral non-perfusion and neovascularization elsewhere (NVE). The serum (QuantiFERONTB Gold) and the tuberculin skin test were the only positive investigations. The FFA showed clear leakage from NVE and peripheral ischemia, Figure 5. The ischemic area treated with argon laser then she received full anti-tuberculous treatment for nine months covered with oral steroids for the first three months to prevent reactivation. No recurrence was seen.
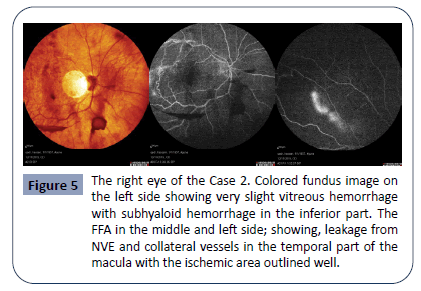
Figure 5: The right eye of the Case 2. Colored fundus image on the left side showing very slight vitreous hemorrhage with subhyaloid hemorrhage in the inferior part. The FFA in the middle and left side; showing, leakage from NVE and collateral vessels in the temporal part of the macula with the ischemic area outlined well.
Case number 3
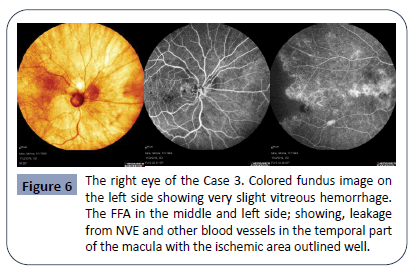
A 60 years old shepherd, myopic male, smoker presented with sudden onset of floaters in the OD eye. A review of systems was normal for all medical and surgical issues with no history of using any drug. Ocular examinations showed the BCVA 6/24 OD and 6/12 OS. The AS and IOP were normal except mild cataracts OU; the posterior segment examination revealed a very mild vitreous hemorrhage with the peripheral non-perfusion area. Again (QuantiFERON-TB Gold) and the tuberculin skin test were positive. Fundus fluorescein angiography (FFA) showed peripheral ischemia, telangiectasia, and leakage, Figure 6.
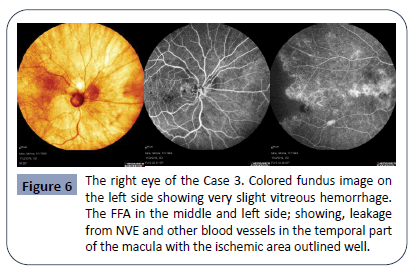
Figure 6: The right eye of the Case 3. Colored fundus image on the left side showing very slight vitreous hemorrhage. The FFA in the middle and left side; showing, leakage from NVE and other blood vessels in the temporal part of the macula with the ischemic area outlined well.
The patient treated with argon laser and was given full antituberculous therapy covered with oral steroids. One month later, the patient came with deterioration in his vision in the affected eye after stopping steroids abruptly by himself. We re-started the oral steroid, and his vision improved gradually over one month. In all cases, systemic workup carried out to rule out any possible causes. Complete blood picture (CBP) and ESR, hemoglobin (Hb) electrophoresis to rule out sickle cell disease. Serological tests, including antinuclear antibody (ANA) for systemic lupus erythematous, C-reactive protein (CRP) for sarcoidosis, and VDRL for syphilis; all were normal in all patients. Chest X-ray was normal in all of them.
Discussion
There is a list of the differential diagnosis for Eales' disease, but to reach the Eales diagnosis, we must exclude other causes. The natural course of the disease, the clinical presentation, and the FFA findings make the Eales disease confirmed [7]. The differential diagnosis of the Eales disease is a long list of vasculitis. It simply includes primary venous occlusion, diabetic retinopathy, Behcet's disease, sarcoidosis, syphilis, Lyme, multiple sclerosis, Susac disease, collagen diseases, and hemoglobinopathy.
There are neither specific nor sensitive laboratory tests for the disease, but they help to figure out systemic causes of occlusive retinal vasculopathy. Eales disease thought to be a primary noninflammatory disease of the peripheral vascular wall [4]. But a robust association between Eales disease and tuberculosis has been reported by Biswas et al [3]. Even the Tuberculin skin test (PPD), its role in diagnosing Eales disease is questionable [8].
The treatment strategy was applied according to the stage of the disease. For the early disease, steroids, anti-tubercular therapy and vascular endothelial growth factor (VEGF) inhibitor injections might need [4]. In the late stage, the non-perfused retinal area treated with scattered argon laser.
The vitreous hemorrhage was not so severe in our cases and almost all come for the complaint of floaters rather than decreased visual acuity to consider anti-VEGF like what is present in the literature.
In the case number one, the patient was on systemic steroids and regular checkups. After three months of the treatment with oral steroids, we found a new ischemic area as an extension of the previous ischemic area. We had consulted our advisor Prof Dr. Nilüfer Yalç?nda?*; she recommended giving the full anti-TB for one year combined with systemic steroids. Also, the new ischemic area treated with scattered argon laser photocoagulation. After completing anti-TB therapy, neither vascular activity nor new ischemic areas detected on FFA. Therefore, we might speculate that the steroid monotherapy in the early phase might have a progressive impact rather than improvement.
In the case number two, the peripheral retinal hole had misled the first ophthalmologist to think about Eales disease, possibly who had correlated the vitreous cells due to both retinal pigmented epithelium and the avulsed blood vessel on the operculum, secondary to the acute posterior vitreous detachment. Worsening the same symptom had made the patient to re-consult, a meticulous retinal findings were relevant with the Eales disease. However, the results were relevant to the Eales disease. We think the hole is not related to the Eales disease; it is just a coincidental event since there is no mechanical traction to do so. Therefore, patients with high risk to exposure to tuberculosis such as medical staff, floaters with pigmented vitreous cells should be taken into consideration even if there is a break or hole in the retina in order not to miss comorbid conditions.
The case number three, a typical Eales disease patient but a unilateral one, was given a full anti-TB therapy covered by oral steroids. The patient suddenly stopped the oral steroid without notice, and a severe vitreous hemorrhage happened. It was thought that this was because of, Jarisch–Herxheimer reaction, as shown by Ganesh et al [11]. We re-started the oral steroids with the head positioning, and the hemorrhage resolved gradually over two months. Therefore, the systemic steroid is a vital conjunction therapy with anti-TB therapy and sudden withdrawal can cause recurrence of the disease.
Conclusion
The diagnosis of Eales disease is an exclusion diagnosis. The natural course, clinical picture and the FFA findings of the illness make the diagnosis possible. Should be treated with full antituberculous therapy plus a short course of systemic corticosteroids. Patients at risk to predispose to tuberculosis need particular concern when presented with vitreous hemorrhage. Presumed tuberculous retinal periphlebitis in Eales disease should be treated with full anti-TB therapy plus a short course of systemic corticosteroids. Steroid monotherapy causes progression of the disease and sudden steroid withdrawal results in reactivation.
Acknowledgment
The author would like to express his heartfelt gratitude to Prof. Dr. Nilüfer Yalç?nda? in School of Medicine, Ophalmology Department, Ankara University Medical Faculty Vehbi Koç Eye Hospital-Ankara-Turkey, for her support and guidance
Declarations
Funding: None
Conflict of interest: None declared
28437
References
- Nicolcescu A, Mocanu C, Dinu L, Olaru A, Ionete M, et al. (2017) Unilateral Eales' disease a case report. Rom J Ophthalmol 61: 144-149.
- Ivanescu R, Ivanescu C, Januschowski K, Ivanescu A (2018) Progression of Eales' disease post-partum and long-term follow-up: a case report. Journal of medical case reports 12: 310.
- Biswas J, Ravi RK, Naryanasamy A, Kulandai LT, Madhavan HN (2013) Eales' disease - current concepts in diagnosis and management. J Ophthalmic Inflamm Infect 3: 11.
- Calugaru D, Calugaru M, El Ghali C (2017) Eales disease in a young adult man Case report. Rom J Ophthalmol 61: 306-309.
- Tiu RY, Arroyo MH (2018) Eales disease: A case report. Ophthalmol Case Rep 2: 8-11.
- Nada M, Qanoongo S, Singh SV, Khurana AK (2017) A rare presentation of exudative macroaneurysms in unilateral Eales' disease. Nepalese journal of ophthalmology : a biannual peer-reviewed academic journal of the Nepal Ophthalmic Society : NEPJOPH 9: 95-98.
- Lauer AK, Lim JI, Tripathy K, FRCS (Glasgow), Shah VA (2018) Eales Disease. American Academy of Ophthalmology.
- Das T, Pathengay A, Hussain N, Biswas J (2010) Eales' disease: diagnosis and management. Eye 24: 472-82.
- Biswas J, Therese L, Madhavan HN (1999) Use of polymerase chain reaction in detection of Mycobacterium tuberculosis complex DNA from vitreous sample of Eales' disease. The Br J Ophthalmol 83: 994.
- Madhavan HN, Therese KL, Gunisha P, Jayanthi U, Biswas J (2000) Polymerase chain reaction for detection of Mycobacterium tuberculosis in epiretinal membrane in Eales' disease. Investigative ophthalmology & visual science 41: 822-825.
- Ganesh SK, Abraham S, Sudharshan S (2019) Paradoxical reactions in ocular tuberculosis. J Ophthalmic Inflamm Infect 9: 19.