Keywords
Down syndrome; Neurosensorimotor reflex integration; Reflex pattern; Developmental disabilities
Introduction
Down syndrome is caused by chromosome 21 abnormalities and is the most commonly identified genetic form of intellectual developmental disorder [1]. The prevalence of Down syndrome appears to be increasing, and current estimates are that about 1 in 700 live births are affected. A number of morphological, health, and neurodevelopmental disorders are associated with Down syndrome. Most children with Down syndrome have reduced muscle strength and tone (hypo-tonicity), excessive/hyper-motor rotation range in joints, and other neurodevelopmental, motor, and cognitive deficiencies [2]. Down syndrome children also have other developmental disabilities, including delayed psychomotor development, learning disabilities, deficient communication skills, and neurobehavioral and psychiatric problems that manifest as behavioral problems. Behavioral problems include aggression, disruptive behavior, attention deficit disorders, and obsessive-compulsive disorders [3]. While improvements in medical care have led to increased life expectancy for those with Down Syndrome [3], therapies for cognitive disabilities often emphasize pharmacologic strategies [4]. Consequently, there is a need for alternative or complementary therapies for addressing the neurodevelopmental deficiencies of children with Down syndrome.
Neurosensorimotor Reflex Integration (NRI) therapeutic modality is a novel and non-invasive method of improving developmental delays and central nervous system function in children with a variety of developmental disabilities [5]. This method addresses disorders with a neurologic component, and it is based on the concept that unconditioned reflexes are not static and facilitate adaptation to the external environment, while becoming the foundation for physical, emotional, and cognitive development [6,7]. Unconditioned reflexes, such as Babkin Palmomental, Babinski, Spinal Galant, and Perez are innate, genetically-based traits that are required for survival by all individuals [8]. In contrast, conditioned reflexes, are learned voluntary responses that require recruitment of unconditioned reflexes [9-13]. Conditioned reflexes such as Leg Cross Flexion-Extension, Bauer Crawling, and Symmetrical Tonic Neck are the basis for most unconscious habits and skills [6,9].
An assumption of the NRI therapeutic modality is that if the reflex arc of sensory input, brain processing, and motor response is complete, and the various reflexes are neurologically mature (myelinated), then physical, emotional and cognitive functions will function normally [12,14]. Alternatively, emotional outbursts, cognitive deficiencies, or atypical movement patterns may occur if there are deficiencies in the interpretation of sensory information or motor responses are abnormal. This appears to be true for autism, where sensory disorders appear to be more frequent and prominent than in children with normal development [15]. Motor disorders are also present in autistic children at birth, and these disorders may be useful for diagnosing autism at a young age [16,17]. The NRI therapeutic modality considers reflex deficiencies as diagnostic of developmental pathology also in children with Down syndrome and other developmental disabilities, as well as clinical targets for correcting deficiencies that can favor improved behavior, emotional stability, and physical control. It also promotes the importance of an early intervention program.
The NRI Assessment separately evaluates 24 basic reflexes that were empirically selected from well-established reflexes [5,16,17]. This evaluation is based on measurement of motor responses because direct measurement of sensory and brain processing is not currently possible. Each reflex receives a single score on a continuous scale of 0-4 using the sum of scores for five parameters: 1. direction of motor or postural response, 2. sensory-motor coordination in a reflex pattern, 3. intensity or strength, 4. response time and its duration, and 5. symmetry [5,16,17]. Clinically, each reflex evaluation is used to develop an individualized, home exercise program that is intended to correct dysfunctional reflex function. Individualized exercise programs are established based on the patient’s reflex deficiencies. These programs are developed at NRI training conferences where patients are assessed and parents or caregivers are trained to perform neurosensorimotor exercises at home. The conferences offer six different neurosensorimotor training sessions each day. Although neurosensorimotor training sessions are selected based on the patient’s needs (Appendix 1), each training session is based on the same neurosensorimotor concepts.
Improved reflex scores following use of Neurosensorimotor Reflex Integration has anecdotally been observed to correspond with improved behavior, emotional stability, and/or physical control. Consequently, improved reflex scores are objective measures of improved function following use of the NRI programs. Statistical comparisons of improved reflex scores require integration of 24 reflex evaluations into a single score (Zc) that represents overall function. Therefore, an ANOVA was developed that incorporates reflexes grouped by functional body movement planes [18].
This study of 54 children with Down syndrome documents the effectiveness of NRI for improving the functioning of children with Down syndrome. Improved reflex scores were used as objective measures for before and after comparisons. This study evaluates the efficacy of NRI for improving the functions of the sensory motor sphere of children with developmental deficiencies.
Material and Methods
Study design
This study documented improvement in 54 children (6 months to 18 years old) with Down syndrome; 21 females (9 children of 0-5 years, 8 children of 6-12 years, and 4 children of 13-18 year old age) and 33 males (12 children of 0-4 years, 11 - of 6-12 years, and 9 of them of the age of 13-18). 50 children were diagnosed by genetic analysis as trisomy disorder and 4 as mosaic disorder (mixed). The level of severity of disability was determined based on their diagnosis of the IQ as the main criteria accepted in medical and psychological evaluations [19-21]. 33 children with Down Syndrome were checked as follows: 13 children with mild disorder (IQ: 50-70), 16 of moderate disorder (IQ: 35-50), and 4 children with severe disorders (IQ: 20-35). 21 children other were not checked for levels of severity of the symptoms due to the challenge of testing their intellectual retardation at their younger ages.
The research group of children (Study Group) attended at least one NRI training conference held during the 2011 and 2012 calendar years versus the control group of 30 individuals with Down Syndrome (the same age of 6 months to 18 years old; females and males) (Control Group 1) and also individuals with neurotypical development (Control Group 2). Conferences were held in Warsaw, Poland; San Francisco, New Jersey, and Florida, USA; and Vancouver, Canada. Group sizes at these multiple day conferences were 12-24 participants. Inclusion criteria included: completion of a Reflex Parameters Assessment before (pre-test) and after (post-test) attendance at a training conference (8 days: 4 days of intense training, one day rest, followed by another 4 days of training), and completion of six 50-minute training sessions during a training conference (total 64 therapy hours). Training session topics included: Neurostructural Reflex Integration; Tactile Integration; Dynamic and Postural Reflex Re-patterning; Visual and Auditory Reflex Integration and Oral-Facial Reflex Integration; Proprioceptive and Vestibular Skills Development, Lifelong Reflex Integration; and Archetype Movement Integration. Receipt of informed consent was received from all participants’ parent or legal guardian. Assessments were conducted and therapy administered by Specialists or Core Specialists in Training who have successfully completed a specific set of courses and clinical hours in NRI.
The research also presents study data on a control group of 46 individuals with Down syndrome (Control Group 2, the same age of 6 months to 18 years), who did not go through NRI training. Among them there were 19 females (9 children of 0-5 years, 6 children of 6-12 years, and 5 children of 13-18 year old age) and 27 males (11 children of 0-4 years, 9 children of 6-12 years, and 9 children of 13-18 years). Forty-one children were diagnosed as trisomy disorder and five as mosaic disorder (mixed). The severity levels of 26 other children with Down syndrome was as follows: 13 children with mild disorder (IQ: 50-70), 10 moderate disorder (IQ: 35-50), and 3 children with severe disorder (IQ: 20-35). Twenty children were not checked for symptom severity levels due to their younger age. The pre- and post-test of reflex patterns were carried out within the same time frame of 9 days.
The third group that participated in research were children with neurotypical development (780 individuals from 6 to 19 years; 421 females and 359 males [some of this data was reported at international conferences and was published previously]); 356 children of 0-5 years, 265 children of 6-12 years, and 159 children of 13-18 years). They did not go through the NRI training. The pre- and post-test of reflex patterns were carried out within the same time frame of 9 days.
Ethical approval
Institutional Review Board (IRB) approval was granted by the New England IRB (85 Wells Avenue, Suite 107, Newton, MA 02459) (IRB ll-173). The New England Institutional Review Board is a central institutional review board for sponsors, CROs and individual researchers across North America (https://www.neirb. com). The IRB ensures the safety of human subjects in clinical trials by committing a thorough and ethical IRB review process. The New England IRB is registered with both the FDA and the Office for Human Research Protections (OHRP) under IORG Number IORG0000444, and has Full Accreditation status from the Association for Accreditation of Human Research Protection Programs (AAHRPP). Adverse effects (new or worsening medical conditions of any kind) were promptly investigated and reported to the IRB. All participants were assigned codes to protect anonymity.
Measures
The primary outcomes of interest were changes in the reflex patterns of children with Down syndrome. Reflex Pattern Assessments were conducted prior to (pre-test) and after conferences (post-test) and compared. Evaluations of motor and cognitive patterns considered the child’s age, neurologic abnormalities, and status of inborn reflex patterns. Briefly, this entailed grading 24 reflexes (Diagnostic Quality Features coded X1-X24) using five criteria: reflex pattern (or sensory-motor circuit), direction of a response (or movement), strength of reaction, time of reaction, and symmetry. Grades were assigned on a continuous scale of 0-4, with 4 indicating full display of a parameter, and 0 indicating the parameter’s absence. This results in a maximum score of 20 for each reflex (Table 1). Summary scores of 11-20 represent varying degrees of partially or fully integrated reflex patterns, scores 0-9 reflect varying degrees of abnormal development, and scores of 10 to 11.75 are marginal. Scores 16-17.75 represent the norm. Reflex patterns were further categorized according to body movement planes, with eight reflex patterns each corresponding to sagittal, horizontal, and dorsal body movement planes [5].
| Normal Function |
Dysfunction/Pathology |
| Points |
Level of reflex integration |
Points |
Level of reflex dysfunction |
| 20 |
Full / Complete integration |
10-11.75 |
Marginal pathology and dysfunction |
| 18-19.75 |
Mature and integrated |
8-9.75 |
Improper light dysfunction |
| 16-17.75 |
Properly developed-normal |
6-7.75 |
Dysfunction |
| 14-15.75 |
Proper, but low level of development |
4-5.75 |
Severe dysfunction |
| 12-13.75 |
Proper, but very low level of development |
2-3.75 |
Pathology |
| 10-11.75 |
Marginal pathology and dysfunction |
0-1.75 |
Severe pathology |
Table 1: Clinical assessments of Reflex Pattern Assessment scores.
Statistical methods
Results of Reflex Pattern Assessments in children with Down syndrome were analyzed based on the multivariable function z=f(x) of directly non-observable phenomena [18]. Briefly, this function estimates the level of the reflex pattern integration Z as a function of the grading reflex patterns X1, X2,..., X24, with the assumption that this is a linear function. Consequently, variable ZS (sagittal) summarizes information from the first eight reflex patterns X1, X2,..,X8, variable ZH (horizontal body plane) summarizes the information from the second eight reflex patterns X9, X10,..,X16, and variable ZD (dorsal) summarizes the last eight reflex patterns X17, X18,..,X24. The level of the reflex pattern integration (ZC) is estimated by the measured reflex patterns (X1, X2,..., X24). In this case, instead of taking the 24 values with each of the scores (0 to 20) for each patient, we determine three values of reflex pattern integration by body plane symmetry and/or one value of the reflex pattern integration level z for values between 0 and 1. Mean values of ZC, ZS, ZH, and ZD were compared before and 11 days after participating in the NRI program using an ANOVA test developed for this type of analysis (IBM SPSS Statistics Grad Pack 22.0). Results were considered statistically significant where p<0.01 and not significant at p>0.05.
Part of statistical evaluations were performed also with the Mann- Whitney U-test, using Statistica (version 6.0; Stat Soft Inc, Tulsa, OK, USA). P values (M ± SD) less than 0.001 were considered significant and not significant at p>0.05.
Results
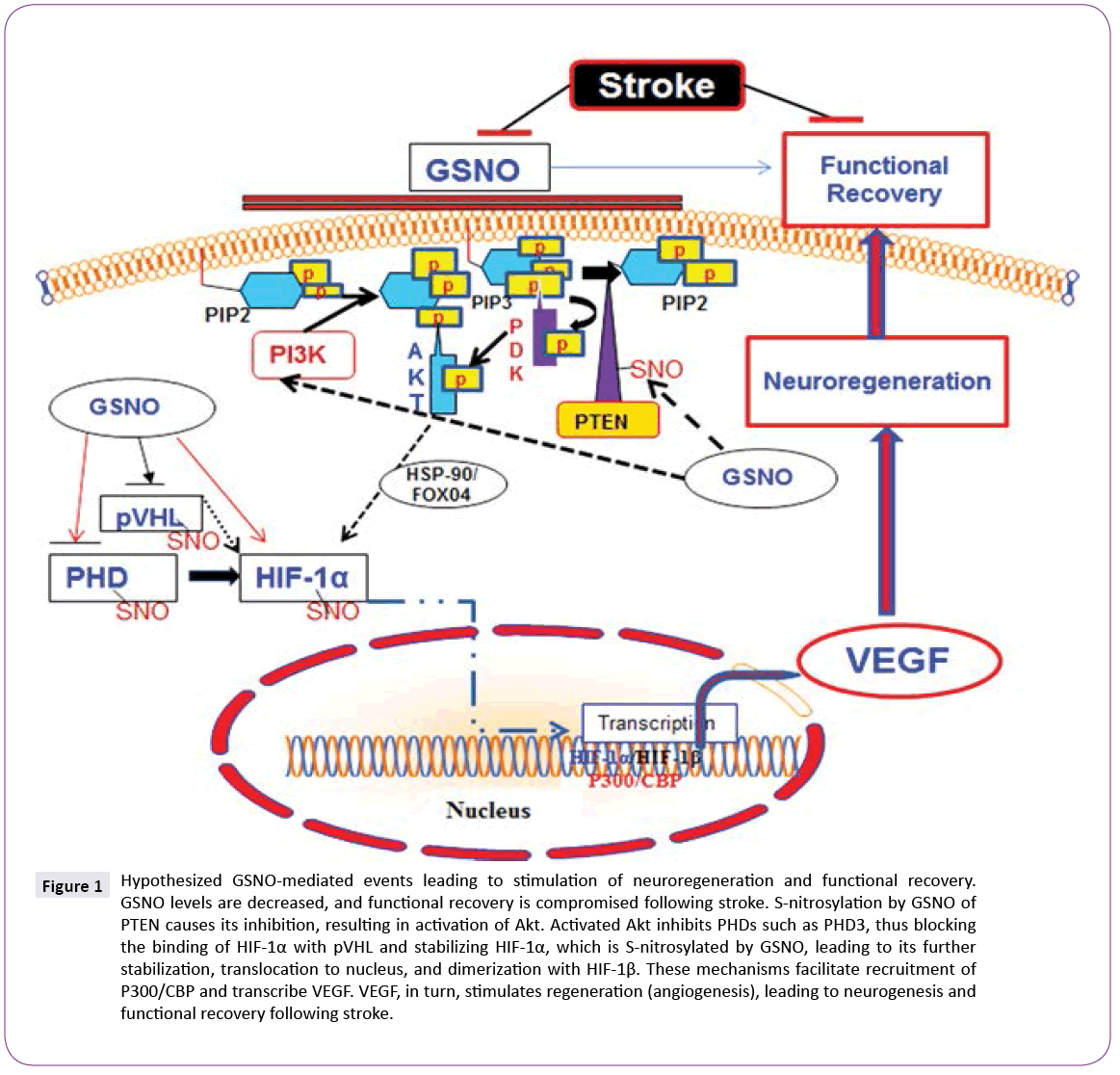
Initial reflex scores of children in Study Group ranged from severe dysfunction (4.5) to low levels of development (12) (Table 2). Significant number of their reflexes - 83,3% - showed substantial improvement after completion of NRI - Neurosensorimotor reflex integration -programs (Table 2), though not to the level of development comparable to that of children with typical development (Table 2 and Figure 1). 16,7% of reflex patterns (the Automatic Gait, Hands Supporting, Flying and Landing and Pavlov Orientation) didn’t show the statistical significance though positive changes were noticed particularly, in such patterns as: the Automatic Gait pattern - in more balanced manner and speed of walking; the Hands Supporting - movement orientation in space, strength of muscles. The means of all reflexes summarized by body plane symmetry (Z values) increased after completion of the NRI program, as did the cumulative ZC value (Table 3).
| Diagnostic Quality/ Feature |
Body Movement Plane |
Reflex |
Results of Assessment |
| Study Group (54 individuals with Down Syndrome) |
Control Group 1 (46 individuals with Down Syndrome) |
Control Group 2 (780 individuals with neurotypical development |
| Pre-test: Before Program |
Post-test:
After Program |
Pre-test |
Post-Test
(in 9 days) |
Pre-test |
Post-Test |
| X1 |
S |
Robinson Hands Grasp (RGR) |
6,4 ± 0.5 |
8,2 ± 0.7* |
6,2 ± 0.4 |
6,3 ± 0.3 |
17 ± 0.7 |
17 ± 0.7 |
| X2 |
S |
Hands Pulling (HPR) |
8,4 ± 0.4 |
9,2 ± 0.3* |
8,1 ± 0.3 |
8,2 ± 0.5 |
16 ± 0.5 |
16,1 ± 0.8 |
| X3 |
S |
BabkinPalmomental (BPR) |
4,5 ± 0.5 |
5,4 ± 0.3* |
4,5 ± 0.4 |
4,4 ± 0.6 |
16 ± 0.8 |
15,8 ± 0.9 |
| X4 |
S |
Babinski (BR) |
6,7 ± 0.4 |
7,3 ± 0.7* |
6,7 ± 0.4 |
6,6 ± 0.3 |
16,5 ± 0.8 |
16,5 ± 1.2 |
| X5 |
S |
Leg Cross Flexion-Extension (LCFER) |
5,5 ± 0.6 |
6,9 ± 0.7* |
5,3 ± 0.2 |
5,3 ± 0.3 |
17 ± 0.9 |
17,1 ± 0.7 |
| X6 |
S |
Asymmetrical Tonic Neck (ATNR) |
6,7 ± 0.3 |
7,4 ± 0.3* |
6,4 ± 0.3 |
6,3 ± 0.2 |
15 ± 0.7 |
15 ± 0.9 |
| X7 |
S |
Abdominal (AR) |
8,2 ± 0.6 |
10,4 ± 0.4* |
8,4 ± 0.6 |
8,3 ± 0.5 |
16 ± 1.0 |
16,1 ± 0.9 |
| X8 |
S |
Bonding (BR) |
12 ± 0.3 |
13,2 ± 0.7* |
11,6 ± 0.5 |
8,9 ± 0.7 |
15,5 ± 0.7 |
15,5 ± 0.8 |
| X9 |
H |
Thomas Automatic Gait (TAGR) |
8,8 ± 0.3 |
9,3 ± 0.4 |
8,5 ± 0/4 |
8,6 ± 0.3 |
17,5 ± 0.9 |
17,4 ± 1.3 |
| X10 |
H |
Bauer Crawling (BCR) |
6,5 ± 0.5 |
9,4 ± 0.7* |
6,6 ± 0.3 |
6,5 ± 0.5 |
15,5 ± 0.6 |
15,5 ± 0.8 |
| X11 |
H |
Moro Embrace (MR) |
11 ± 0.6 |
13,2 ± 0.7* |
11,2 ± 0.7 |
10,9 ± 0.5 |
15,5 ± 0.6 |
15,5 ± 0.8 |
| X12 |
H |
Fear Paralysis (FPR) |
12 ± 0.5 |
13,4 ± 0.7* |
11,8 ± 0.5 |
11,9 ± 0.6 |
14,5 ± 0.5 |
14,6 ± 0.7 |
| X13 |
H |
Hands Supporting (HSR) |
8,3 ± 0.3 |
8,9 ± 0.4 |
8.1 ± 0.3 |
8,2 ± 0.2 |
15,5 ± 0.7 |
15,5 ± 0.9 |
| X14 |
H |
Segmental Rolling (SRR) |
7,2 ± 0.4 |
8,1 ± 0.3* |
7,4 ± 0.4 |
7,2 ± 0.5 |
15 ± 0.8 |
15,4 ± 1.2 |
| X15 |
H |
Landau (LR) |
6,4 ± 0.4 |
7,2 ± 0.2* |
6,1 ± 0.3 |
6,1 ± o.4 |
15 ± 0.8 |
15,1 ± 1.1 |
| X16 |
H |
Flying and Landing (FLR) |
5,2 ± 0.4 |
5,8 ± 0.5 |
4,8 ± 0.4 |
4,9 ± 0.5 |
14,5 ± 0.7 |
14,5 ± 0.9 |
| X17 |
D |
Trunk Extension (TER) |
8,2 ± 0.3 |
8,8 ± 0.2* |
7,8 ± 0.4 |
7,9 ± 0.6 |
16 ± 0.7 |
16,2 ± 0.8 |
| X18 |
D |
Symmetrical Tonic Neck (STNR) |
6,3 ± 0.7 |
8,4 ± 0.6* |
6,4 ± 0.5 |
6,5 ± 0.6 |
16 ± 0.6 |
15,8 ± 0.9 |
| X19 |
D |
Spinal Galant (SGR) |
8,3 ± 0.7 |
11,2 ± 0.8* |
8,5 ± 0.5 |
8,4 ± 0.6 |
15 ± 0.9 |
15 ± 1.2 |
| X20 |
D |
Spinal Perez (SPR) |
11 ± 0.4 |
12,3 ± 0.8* |
10,4 ± 0.9 |
10,2 ± 0.8 |
16 ± 0.7 |
16,1 ± 1.2 |
| X21 |
D |
Tonic Labyrinthine (LTR) |
9,2 ± 0.7 |
11,2 ± 0.6* |
9 ± 0.7 |
8,9 ± 0.5 |
16 ± 0.9 |
16,1 ± 1.1 |
| X22 |
D |
Foot Tendon Guard (FTGR) |
8,1 ± 0.6 |
10 ± 0.5* |
8 ± 0.4 |
7,9 ± 0.5 |
15,5 ± 0.8 |
15,3 ± 1.2 |
| X23 |
D |
Spinning (SR) |
8,3 ± 0.8 |
12,4 ± 0.7* |
8 ± 0.6 |
8,2 ± 0.5 |
15 ± 0.9 |
15,1 ± 1.7 |
| X24 |
D |
Pavlov Orientation (POR) |
6,6 ± 0.2 |
6,8 ± 0.3 |
6,7 ± 0.3 |
6,6 ± 0.5 |
18,5 ± 0.7 |
18,5 ± 0.9 |
* Statistical significance P<0.05.
Table 2: Diagnostic Quality Feature (X1-X24), body movement planes (S = sagittal; H = horizontal; D = dorsal), reflexes, and assessments before and after participation in neurosensorimotor reflex integration (NRI) conferences.
| Variables |
Average values and standard deviations for three synthetic variables, ZS (sagittal body plane), ZH (horizontal), and ZD (dorsal) |
Study Group
(54 individuals with Down Syndrome) |
Control Group 1
(46 individuals with Down Syndrome) |
Control Group 2
(780 individuals with neurotypical development |
| Before |
After |
ANOVA |
Before |
After |
ANOVA |
Before |
After |
ANOVA |
| |
Mean |
S.D. |
Mean |
S.D. |
P< |
Mean |
S.D. |
Mean |
S.D. |
P> |
Mean |
S.D. |
Mean |
S.D. |
P> |
| ZC |
0.3924 |
0.1884 |
0.6038 |
0.1790 |
0.001 |
0.4112 |
0.1912 |
0.4213 |
0.1619 |
0.05 |
0.2914 |
0.1782 |
0.3424 |
0.1672 |
0.05 |
| ZS |
0.4083 |
0.1890 |
0.5912 |
0.1940 |
0.001 |
0,3876 |
0.1812 |
0,3576 |
0.1872 |
0.05 |
0.3063 |
0.1680 |
0.2852 |
0.1662 |
0.05 |
| ZH |
0.3861 |
0.1792 |
0.6088 |
0.1754 |
0.001 |
0.4084 |
0.1712 |
0.4102 |
0.1692 |
0.05 |
0.2851 |
0.1572 |
0.2641 |
0.1585 |
0.05 |
| ZD |
0.4135 |
0.2076 |
0.5849 |
0.1853 |
0.001 |
0.3913 |
0.1893 |
0.3818 |
0.1953 |
0.05 |
0.3142 |
0.1265 |
0.3341 |
0.1357 |
0.05 |
Table 3: Participant’s (N = 54; Study Group) average values and standard deviations for three synthetic variables, ZS (Sagittal body plane), ZH (Horizontal), and ZD (Dorsal) that represent functional participant diagnostic characteristics by body plane, as well as a summary value ZC (a mean of ZS, ZH, and ZD). All values in Study Group are significantly different vs. in Control groups.
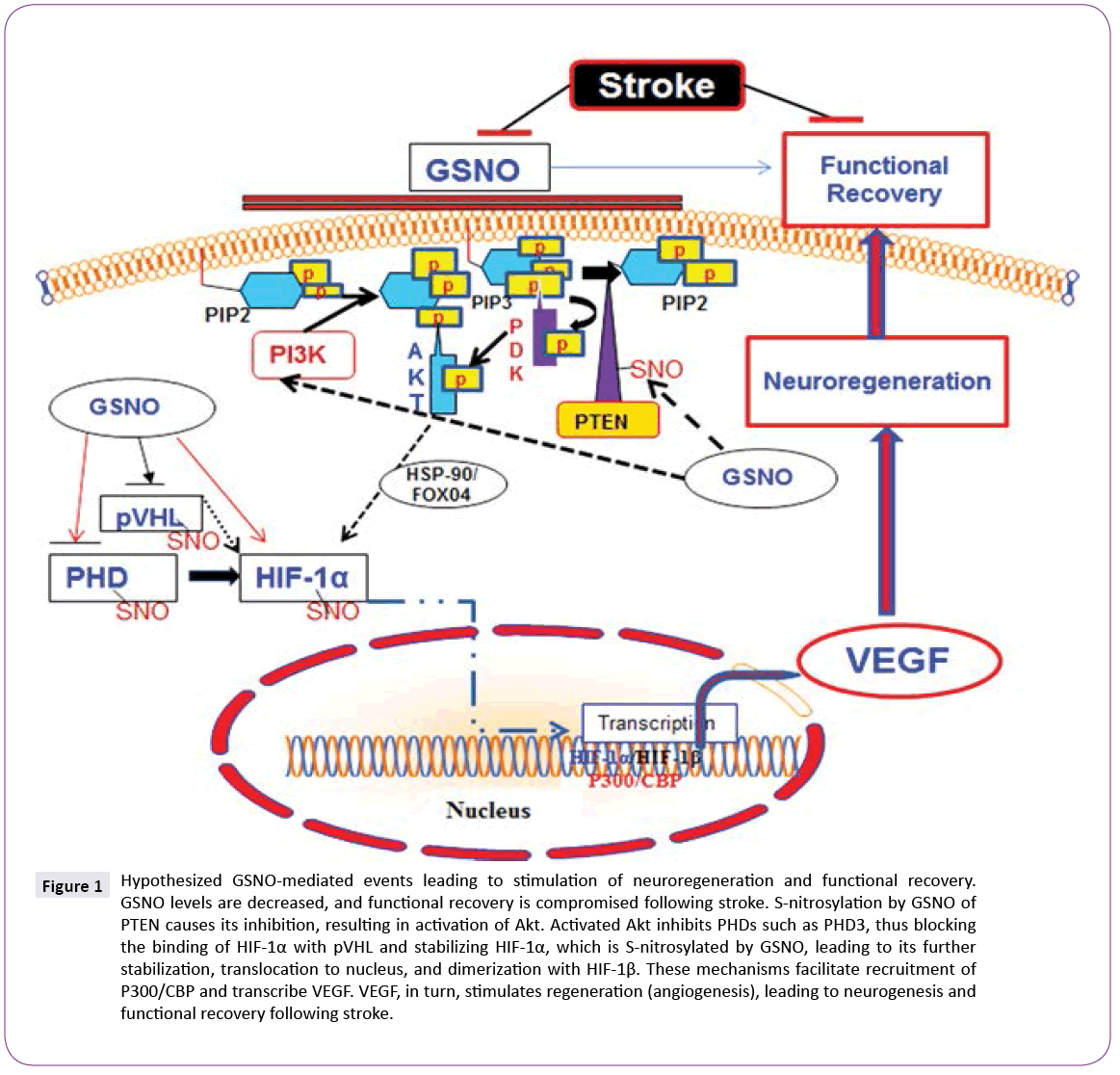
Figure 1: Levels of reflex (Diagnostic Quality Features X1–X24) development/integration for children with Down syndrome in Study Group before and after the MNRI - neurosensorimotor reflex integration program.
Analysis of reflex patterns in children in the Control Group 1 (with Down syndrome) that did not go through the NRI training reveals that there is no positive dynamics (there is no statistical significance - P>0.05) (Tables 2 and 3). The same result is noted towards children with neurotypical development - there are no changes in their reflex dynamic when NRI intervention is not proposed (Table 3).
Also an additional comparative analysis of the improvement of the reflex function dynamic in children with Down syndrome with different level of severity of their disability (A-mild disability, B-moderate, C-severe) has shown that the changes in reflex patterns in every of these sub-groups were statically significant (Table 4), while in Control group such a change has not been occurring (P >0.05), which means that every sub-group in Study Group benefited from the NRI therapy. Still clinic observation and the points for reflex patterns level show that children with severe disability have lower level of development of reflex patterns, and would need longer term work with the use of the NRI Program.
| Groups |
Results of reflex assessment in children with Down syndrome with different levels of disability (with diagnosed IQ) |
| |
Total in research (P<0.001) |
Number/%
(IQ is known) |
A. Mild disability
(IQ: 50–70) |
B. Moderate
(IQ: 35–50) |
C. Severe disability (IQ: 20–35) |
| |
|
Pre-test |
Post- test |
No/ % |
Pre-test |
Post- test |
No/ % |
Pre-test |
Post- test |
No/ % |
Pre-test |
Post- test |
| Study Croup |
54/ 100% |
7.9 ± 0.5 |
9.35 ± 0.61 |
33/ 61.1% |
13/ 24.1% |
9.8 ± 0.4 |
11.25 ± 0.56 |
16/ 29.6% |
8.2 ± 0.4 |
9.6 ± 0.5 |
4/ 7.4% |
5.7 ± 0.36 |
7.2 ± 0.42 |
ANOVA
P |
<0.05 |
|
ANOVA
P |
<0.05 |
ANOVA
P |
<0.05 |
ANOVA
P |
<0.05 |
| Control group 1 |
46/ 100% |
7,77 ± 0.53 |
7,63 ± 0.4 |
26/ 56.5% |
13 / 28,3% |
9.6 ± 0.7 |
9.7 ± 0.81 |
10/ 21.7% |
8.1 ± 0.45 |
7.6 ± 0.5 |
3/ 6.5% |
5.6 ± 0.47 |
5.7 ± 0.52 |
ANOVA
P |
>0.05 |
|
ANOVA
P |
>0.05 |
ANOVA
P |
>0.05 |
ANOVA
P |
>0.05 |
Table 4: Summary of comparative analysis of results of the pre- and post-assessment of reflex patterns (X1-X24) in children with Down syndrome with different levels of disability (in Study Group - before and after participation in neurosensorimotor reflex integration NRI training).
Also an interesting clinical fact is noticed: the progress in correction of the reflex patterns in the Study Group was dependent on age - it was higher in the group of children age 6 months to 5 years, and also in the group of children ages 6 to12 years. It was significant but less in the group of ages 13-18 years, which can be interpreted that the NRI program guarantees higher results in children of 0-12 years of age and emphasizes the importance of early intervention, and that elder children and adults will benefit from longer term work with the NRI tools.
Discussion
Children with Down syndrome have a number of developmental disorders, and there is a need to identify efficacious strategies for improving these children’s functional capabilities. Neurosensorimotor reflex integration (NRI) has been developed as a successful means of assessing and improving the neurological function of children with developmental disorders [22], and anecdotally appears useful for children with Down syndrome. The NRI therapeutic modality is based on the concept that improving the reflexes of children with developmental disorders will improve their sensorimotor, cognitive, and behavioral capabilities and emotional growth. This concept was developed based on Russian and Polish physiological research and anecdotal observations of improved function among children participating in NRI conferences [5,22]. Further support for this concept is evident where improved reflexes result in improved gross and fine motor coordination and postural control [23]. Improved behavior can also occur with NRI training because children learn to regulate involuntary, unconscious, spontaneous motor activity and emotional responses [24]. Therefore, cognition can concurrently improve [25,26]. This study represents an initial step in documenting the efficacy of NRI for improving the functioning of children with Down syndrome and other developmental disabilities.
This study documents that Down syndrome participants' baseline reflexes were largely dysfunctional or pathological, as would be predicted by what is known of Down syndrome and the basis of the NRI Assessment method [5]. Participants’ reflexes (Table 2 and Figure 1) and summarized results of reflex assessment (Table 3) showed improvement in Down syndrome children’s sensorymotor skills following completion of NRI training sessions. Anecdotally, these improvements in motor skills correspond to the participants’ improved cognitive, language, and communication skills, and decrease in behavioral problems. Further evaluation of NRI for improving the functioning of children with Down syndrome and other developmental disorders is in progress.
Comparison of results of children in the Study Group (with Down syndrome) that went through the NRI training Program with results of children (with Down syndrome) in Control Group 1 that did not go through the NRI Program reveals that the level of changes in reflex patterns are statistically significant in the Study Group (P<0.05), versus results in the Control Group, in which the dynamic statistically is not significant (P>0.05) (Tables 2 and 3). This shows a significant positive effect of the work with children with Down syndrome using the NRI Program.
Similarly, the comparison of results in Study Group, Control 1 (both Down syndrome) and pre- and post-test in Control Group 2 of neurotypical children also demonstrates that the changes took place only in the Study Group, where the NRI program was applied (Table 3). This can point out at the fact that correction of reflex patterns in this short length of time happens only, if the specialized program is used; and that there are no any significant changes, if the corrective work is not done - independently of whether the participant is in the group of the development deficit children or neurotypical children.
Also an interesting fact is noted: the progress in correction of the reflex patterns in children in the Study Group was dependent on age - it was higher in the group of children age 6 months to 5 years, and also in the group of children ages 6 to12 years. It was significant but less in the group of ages 13-18 years, which can be interpreted that the NRI program guarantees higher results in children of 0-12 years of age and emphasizes the importance of early intervention.
Additional comparative analysis of the improvement of reflex patterns overall in different sub-groups of children with Down syndrome, depending on severity of their disability, has shown that the changes in every group are statistically significant (Table 4): results of changes in children in Study Group with mild disability (pre-test: 9.8 ± 0.4; post-test: 11.25 ± 0.56), moderate (pre-test: 9.8 ± 0.4; post-test: 11.25 ± 0.56), and severe (pretest: 5.7 ± 0.36; post-test: 7.2 ± 0.42) show p<0.05 compared to results in Control Group of children with Down syndrome with mild disability (pre-test: 9.6 ± 0.7; post-test: 9.7 ± 0.81), moderate (pre-test: 8.1 ± 0.45; post-test: 9.7 ± 0.81), and severe (pre-test: 5.6 ± 0.47; post-test: 5.7 ± 0.52), in which P>0.05. These results mean that children in all three groups had benefited from the NRI techniques program. In contrast, in both Control groups, where the children did not go through the NRI program, the improvement in reflex patterns did not occur: Control Group 1 (children with Down syndrome; p>0.05), and in Control Group 2 (children with neurotypical development; p>0.05). This data validates the long-term clinical observation that improper work of reflex patterns needs specific knowledge and evaluation of parameters of reflex patterns (identify what parameter is poorly developed or dysfunctional, or pathological) and directed correction procedure. The NRI method contains such a procedure with leads to a significant success in sensorimotor development in children with Down syndrome (which was also noticed with other genetic disorders, such as Prader-Willi syndrome, Fragile-X, and equally in cases of other neurodeficits (cerebral palsy, brain damage, autism).
Clinical observation of professionals (OTs, PTs, SPs, special educators, psychologists among others) and parents show that children with Down syndrome after the NRI program improve their balance, postural control, motor programming, planning and control facilitating their coordination of movements, strength, precision, space-time orientation, speed of perception and response, better ‘presence’, easier focusing, better memorizing, and improvement in language development (receptive and expressive).
Conclusions
The NRI program significantly improves the reflex functions of children with Down syndrome (6 months to 18 years old) (n = 54) by improving their sensory-motor integration. This serves as an indication that the neurosensory development and overall functioning of these children are not static and can be improved independently of the genetic roots of the disorder. Consequently, NRI may offer an effective means of improving the overall functioning of children with Down syndrome serve as an exemplary tool for children with other neurodeficits and learning disabilities.
This study also shows that the changes in affected reflex patterns follow after specific NRI therapy intervention; and that the improvement in affected reflex patterns do not happen spontaneously in children that: a) have improper working reflex patterns, and b) did not go through the NRI program. This study shows the importance of intervention therapies that target at corrective work with reflex patterns, the units of nerve system functioning. The authors of this article based on long-term clinical observations consider that the NRI program must serve as a basic start therapy for other types of therapy modalities - physiotherapy, occupational therapy, speech pathology therapy, sensory integration and other.
Comparative analysis of reflex patterns improvement in different groups of children with Down syndrome, depending on severity of their disability based on their IQ (mild, moderate and severe), has shown that the children in all three sub-groups have benefited from the NRI techniques as they have shown significant changes in their reflex pattern functions and sensorimotor sphere. In contrast, in Control groups, where children did not go through the NRI program the changes in reflex patterns were not noticed. This data validates the long-term clinical observation of the fact that poor functioning or dysfunctional reflex patterns need specific treatment tools built on exact knowledge of neurophysiology of a reflex circuit and evaluation of parameters of a reflex pattern (sensory-motor circuit, direction of response, intensity, latency and symmetry), also identification of the level of reflex function/ development (poorly developed or dysfunctional, or pathological) and correction procedure oriented at developmental challenges of children with Down syndrome. The NRI method contains such a procedure with leads to a significant success in sensorimotor development in children of this group of disorder (which was also noticed with other genetic syndromes, such as Prader-Willi, Fragile-X, and equally in cases of other neurodeficits (cerebral palsy, brain damage, autism).
This research further plans to share information concerning the neurophysiological mechanism and biomechanical aspects of a reflex pattern that the NRI program successfully activates though corrective tools using the reflex pattern as the ‘model scheme’ to improve the reflex circuits parameters and sensory-motor patterns functions in children with Down syndrome; particularly, to show the ways how to target the neuro-sensory-motor components of a reflex pattern and other automaticity in order to support the maturation and strengthen the lower motor neurons functions and subcortical structures of the brain for support of higher executive functions, such as postural control, motor coordination, regulation of behavior and emotions, cognitive processes (comparison, analysis, comprehension, language), and personality development.
8109
References
- Sherman SL, Allen EG, Bean LH, Freeman SB (2007) Epidemiology of Down syndrome. Mental Retardation and Developmental Disabilities Research Reviews 13:221-227.
- Souchay C, Guillery-Girard B, Pauly-Takacs K, Wojcik DZ, Eustache F (2013) Subjective Experience of Episodic Memory and Metacognition: A Neurodevelopmental Approach. Frontiers in Behavioral Neuroscience 7:212.
- Weijerman ME, de Winter JP (2010) Clinical practice. The care of children with Down syndrome. European Journal of Pediatrics 169:1445-1452.
- Wiseman FK, Alford KA, Tybulewicz VL, Fisher EM (2009) Down syndrome-- recent progress and future prospects. Human molecular genetics 18:R75-R83.
- Masgutova S, Masgutov D (2012) MNRI Oral-Facial Reflex Integration in Children and Adults with Neurodeficits (Polish version). Warsaw, Poland: ISME.
- Anokhin PK (1973) Systemic analysis of a conditioned relfex. Zhurnalvyssheii nervnoi deiatelnosti imeni I P Pavlova 23:229-247.
- Vygotsky L (2012) Thought and Language. Cambridge, MA: MIT Press books.
- Storozhuk VM, Ziniuk LE (1992) Neocortex neuronal reactions induced by substantiainnominata stimulation in cats. Neirofiziologiia 24:11-20.
- Dudkin KN (2001) I P Pavlov principles of the higher nervous activity--a reliable basis for modern cognitive physiology. Rossii?skiifiziologicheskii? zhurnalimeni I.M. Sechenova / Rossii?skaiaakademiianauk 87:829-846.
- Khananashvili MM(2008) General functional state (tonus) of the brain and conditioned reflexes as the mechanisms of it's regulation. Zhurnalvysshei? nervnoi? deiatelnostiimeni I P Pavlova 58:757-766.
- McIntosh RD, Mulroue A, Brockmole JR (2010) How automatic is the hand's automatic pilot? Evidence from dual-task studies. Experimental brain research 206: 257-269.
- Pavlov PI(2010) Conditioned reflexes: An investigation of the physiological activity of the cerebral cortex. Annals of neurosciences 17:136-141.
- Storozhuk VM, Semeniuk EF (1978) Dynamics of neuronal reactions during elaboration of a conditioned defensive reflex to sound. Neirofiziologiia 10:339-347.
- Konorski J (1970) Pavlov and contemporary physiological psychology. Conditional reflex 5:241-248.
- Rogers SJ, Ozonoff S (2005) Annotation: what do we know about sensory dysfunction in autism? A critical review of the empirical evidence. Journal of child psychology and psychiatry, and allied disciplines 46:1255-1268.
- Krefft P, Teitelbaum O, Fryman J, Maurer RG (2002) Reflexes gone astray in autism in infancy. Journal of Developmental and Learning Disorders 6:15-22.
- Teitelbaum P, Teitelbaum O, Nye J, Fryman J, Maurer RG (1998) Movement analysis in infancy may be useful for early diagnosis of autism. Proceedings of the National Academy of Sciences of the United States of America 95:13982-13987.
- Krefft A (2007) Diagnosis of Functions of Invisible Phenomena (Statistic Mathematic Analysis). Wroclaw, Poland: Oficyna Wydawnicza Politechniki Wroclawskiej.
- Batshaw M (2005) Children with disabilities. (5thedn.). Baltimore [u.a.]: Paul H. Brookes. p. 308. ISBN 978-1-55766-581-2.
- Patterson T, Rapsey CM, Glue P (2013) Systematic review of cognitive development across childhood in Down syndrome: implications for treatment interventions. Journal of intellectual disability research: JIDR57 4: 306-18.
- Reilly C (2012) Behavioural phenotypes and special educational needs: is aetiology important in the classroom? Journal of intellectual disability research: JIDR 56 10: 929-46.
- Pilecki W, Masgutova S, Kowalewska J, Masgutov D, Akhmatova N, et al. (2012) The impact of rehabilitation carried out using the Masgutova Neurosensorimotor Reflex Integration method in children with cerebral palsy on the results of brain stem auditory potential examinations. Advances in Clinical and Experimental Medicine 21:363-371.
- Bernstein N (1997) Bio-Mechanics and Physiology of Movement (Russ.). Moscow, Russia: Moscow-Voroniez.
- Bobath K, Bobath B (1984) The neurodevelopmental treatment. In: Scrutton D (ed.) Management of the Motor Disorders of Children with Cerebral Palsy. Oxford, England: Blackwell Scientific Publications Ltd 6-18.
- Montessori M (1995) The absorbent mind. New York, NY: Henry Holt and Company.
- Piaget J (1976) The grasp of consciousness: action and concept in the young child. Cambridge, MA: Harvard Press.