Padam Simkhada1*, Edwin van Teijlingen2, Gaurav Sharma3, Bibha Simkhada4, John Townend5
1MSc, PhD, Senior Lecturer in International Health, School of Health and Related Research (ScHARR), University of Sheffield, Sheffield & Visiting Professor- Monamohan Institute of Health Science and Nepal Institute of Health Science, Purbanchal University, Nepal & Honorary Lecturer, University of Aberdeen, UK & Visiting Fellow, Bournemouth University, UK.
2MEd, PhD, Professor, School of Health & Social Care, Bournemouth University, Bournemouth, UK & Visiting Professor at Manmohan Memorial Institute of Health Sciences, Purbanchal University, Kathmandu, Nepal
3MBBS, MSc, Fellow in Reproductive Health based at WHO, South East Asia Regional Office, New Delhi, India
4RN, BSc, Dugald Baird Centre for Research on Women’s Health, University of Aberdeen, Aberdeen, AB25 2ZD, Scotland, UK
5PhD, Medical Research Council (UK) The Gambia, PO Box 273, Banjul, The Gambia
*Corresponding Author:
Dr. Padam Simkhada
School of Health and Related Research (ScHARR)
University of Sheffield, Regent Court
30 Regent Street, Sheffield S1 4DA, UK
Tel: 0044 (0) 114 222 0752
E-mail: p.simkhada@sheffield.ac.uk
Keywords
Childbirth, corruption, developing countries, informal payment, obstetric care.
Introduction
Maternal mortality, currently an issue of concern on the international health agenda, remains one of the most important public health problems in developing countries. The most recent global estimate is that 342,900 women died during childbirth in 2008 [1]; over 99% of maternal deaths occur in the developing world [2]. The difference in maternal mortality between higher-income and lower-income countries is greater than any other mortality rate. As most deaths in childbirth are preventable, death of women during childbirth is truly the greatest immoral global inequality. Hence, improving maternal health is one of the eight Millennium Development Goals (MDGs). MDG 5 aims at reducing the maternal mortality ratio (MMR) by three quarters by 2015.
Nepal is one of the poorest countries in the world; in 2008 it ranked 195 out of 210 countries [3] and about 31% of the people live below the poverty line [4]. Poverty is intimately linked to high MMR. The Maternal Mortality Rate in Nepal was estimated as 281 deaths per 100,000 live births [5], and in a recent study conducted in eight districts reported 229 /100,000 live births [6]. Underutilization of health services is one contributing factor as 81% of births take place at home, many without skilled attendance [5]. Inequality in uptake of maternal health services remains a challenge, as evidenced by persistence of inequalities, for example, only 4% of the poorest women deliver their baby in health facilities compared to 55% of the richest [5]. In addition, Nepalese women have low status in society. The low status of women causes low utilization of maternal health care [7,8].
The Government of Nepal has started Maternal Incentive Scheme to encourage women who deliver their baby in hospitals. This incentive scheme was initially introduced in 2005 in 25 least developed districts to cover the cost of their travel to healthcare facilities. It mainly aims to increase coverage of skilled birth attendance [9]. The scheme provides incentives to pregnant women and skilled birth attendants (SBA) and subsidies to health institutions for births assisted by SBAs. The amount is vary geographically, with women having their babies delivered in mountainous, hilly, or flat areas receiving, respectively, NRS (Nepalese Rupees) 1500 (€17.40), Rs1000 (€11.60), or Rs500 (€5.80).
Although there is Maternal Incentive Scheme, households often pay a too large share of the costs of maternity services, or do not seek care because of it [10,11]. Health services are financed in two main ways: through out of pocket user charges and from public expenditure. In Nepal only 6% of the national budget is allocated to health services. People have to spend a significant amount of money on health care from their pocket. Nearly three-fourths of the total budget is met by private sources, mostly out-of pocket [12]. For example, 14% of households, the cost of care is catastrophic, representing over 10% of their total income [13].
Costs including direct fees as well as the cost of transportation, drugs and supplies, multiple demands on women’s time are major obstacles in the maternal health service utilisation in Nepal [14]. Emergency obstetric care is very expensive and hospital deliveries generally are the single most expensive period during pregnancy and these have significant financial implications for the household in terms of expenses at the facility, travel costs and time (including not being able to earn money), even when formal charges are not levied, unofficial and additional costs can occur [15-17].
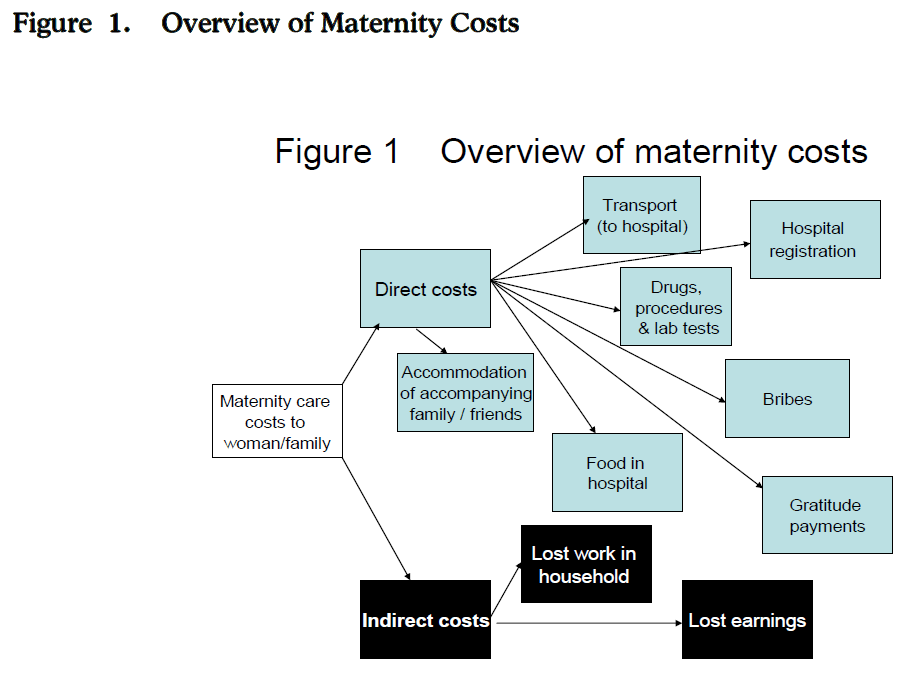
We drew up Figure 1 based on the review of the literature to help highlight the different costs associated with a hospital delivery. Figure 1 shows that for a family maternity care costs comprise (a) direct and (b) indirect costs. Direct costs include formal payments such as costs associated with (a) admission and registration; (b) medical interventions, e.g. blood transfusion; (c) medications and; (d) any investigations and laboratory costs. Informal payments are direct costs related to monetary transactions between patients and staff for services that are not officially sanctioned by the facility [18]. They include payments given in a celebratory fashion (a tip) to welcome the new baby or for (extra) care from hospital support staff, and bribe [19,20].
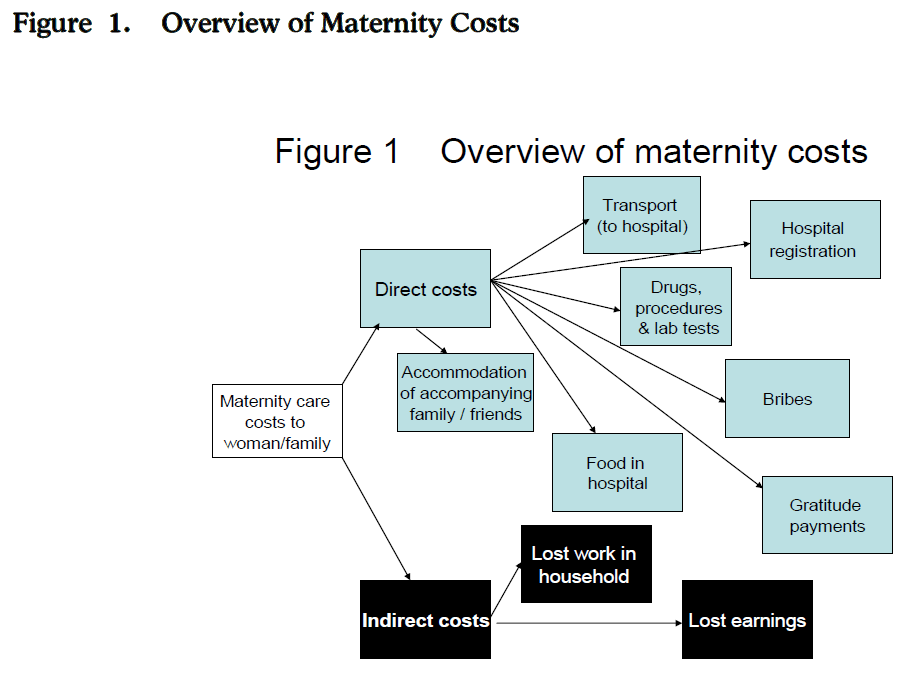
Figure 1: Overview of Maternity Costs
This paper examines (a) the types and amounts of formal and informal payments made for care around birth at a large maternity hospital in Nepal, and (b) underlying factors that affect such out-of-pocket expenses.
Methods
This study used a mixed-method approach; a quantitative survey of women who delivered in the obstetric hospital, followed by qualitative interviews in hospital with a sub-sample of questionnaire participants. The cross-sectional questionnaire survey was conducted over a one-month period in the summer of 2007 with women who had delivered in the hospital after they were formally discharged, but before they left the facility. The survey covered as many as possible of the women in that time period (i.e. those with normal and abnormal labours), with the exception of women who (a) were transferred the Intensive Treatment Unit for complications; (b) delivered elsewhere but came to the hospital afterwards with complications; (c) had negative pregnancy outcomes or seriously ill babies, and (d) suffered mental health problems. The questionnaire included questions on the socio-demographic characteristics of the women who had delivered at the hospital, the costs associated with using maternity services and the decision making process of women (copy of the questionnaire in English is available from the authors).
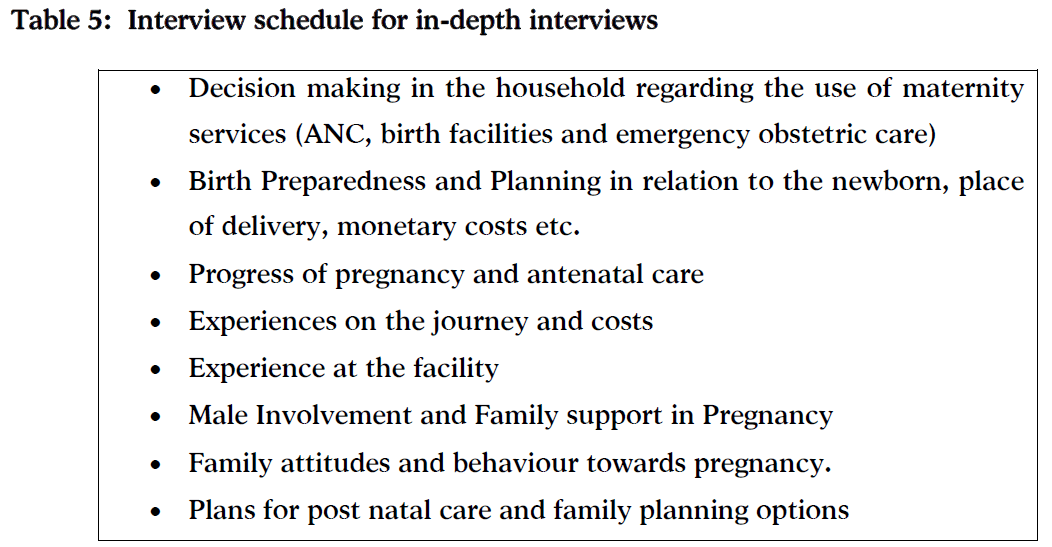
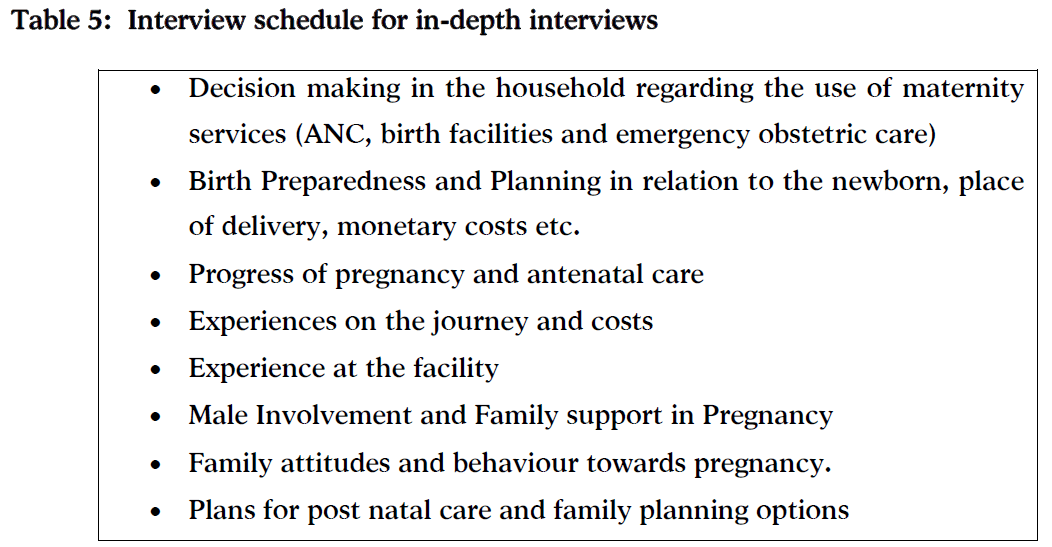
In-depth interviews explored the decision-making process from the perspective of the woman and her family [21]. Women were sampled purposively and interviews were conducted with ten couples to explore key dimensions of interest [22]. The interview schedule included questions on (see Table 5). A pilot study of five interviews with women was conducted prior to the main study to test the questionnaire and the interview schedule [23].
This research was conducted at the government-funded and largest tertiary obstetric hospital (321 beds & approximately 16,000 births p/a) in Kathmandu. The hospital budget of some € 520,000 is supplemented by a modest user charge and is the cheapest hospital for deliveries in Kathmandu Valley.
The questionnaires data were coded, checked, cleaned and entered into SPSS Windows version 15.0. Results of statistical tests are reported to be significant if the p-value was less than 0.05. Logistic regression was used to adjust for the effects of possible confounding factors on the odds of making informal payments. The third author (GS), a native Nepali speaker, transcribed and translated all tape-recorded interviews. The transcripts were coded for key issues by GS. EvT coded a sample of interviews for quality control. Data were organised into different themes and some sections of data fitted more than one theme [24]. Ethical approval was granted by the hospital ethics committee, and participants gave informed consent prior to study.
Results
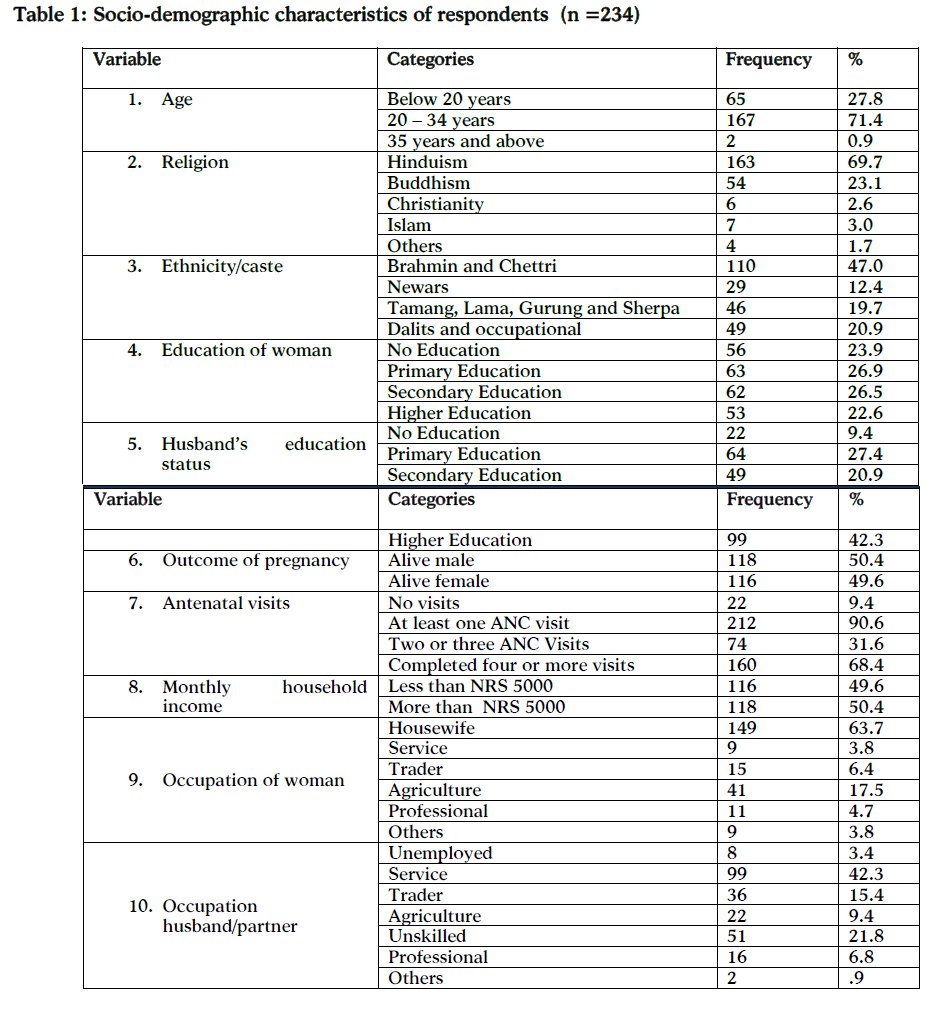
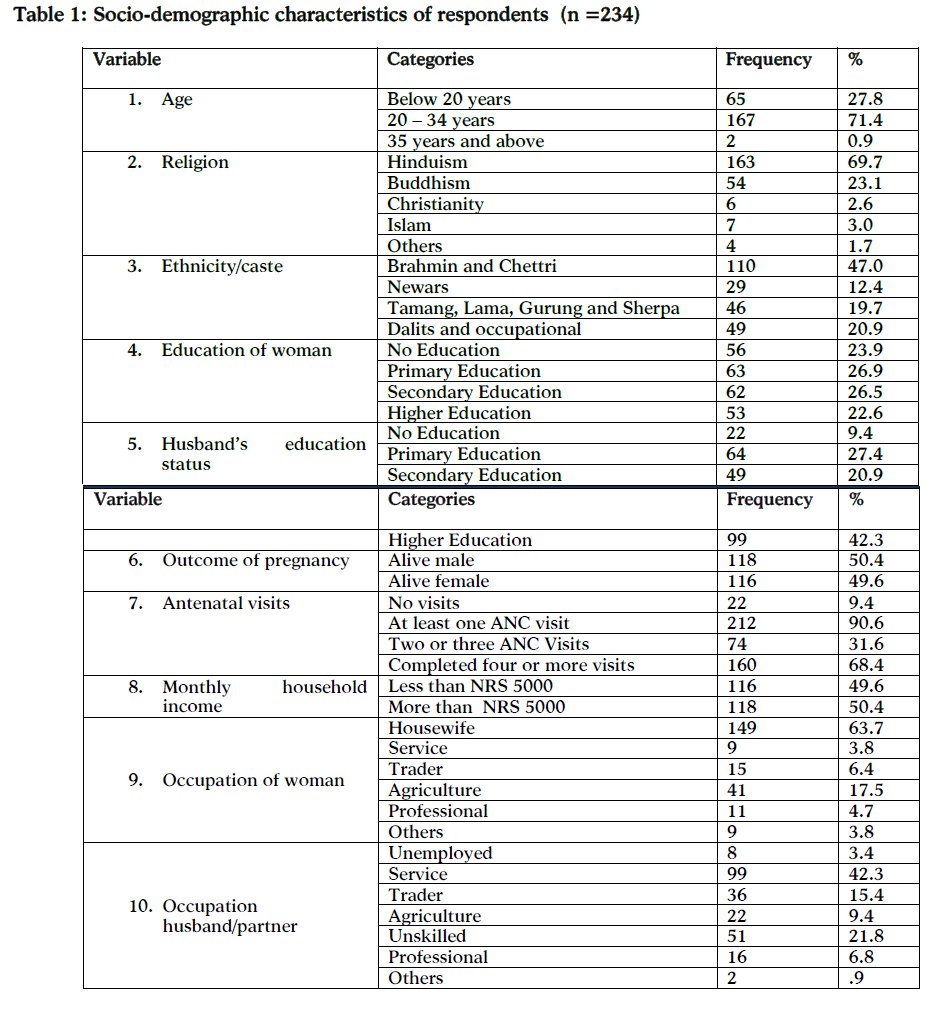
Out of approximately 260 women delivering in the hospital during the study period, 234 completed the questionnaire (response rate about 90%). Table 1 shows that most women (71%) were aged 20-34. The median age was 22 years and the majority was Hindu (70%). The higher castes made up 47% and 64% lived in Kathmandu. Most women had completed four or more ANC visits (median 4.8 visits). Interestingly, 72% lived in nuclear families. Fairly equal proportions of women had completed primary, secondary and higher education. Husbands were more likely to have completed higher education. About half had a monthly income over 5,000 NRS (using June 2007 exchange rate this equals €55.77). Most women were housewives, and two in five of their husbands worked in the service industry. Almost 60% lived in rented accommodation, although 80% owned land. The majority owned a radio/television, however, car and computer ownership was rare.
Women’s expenses in hospital
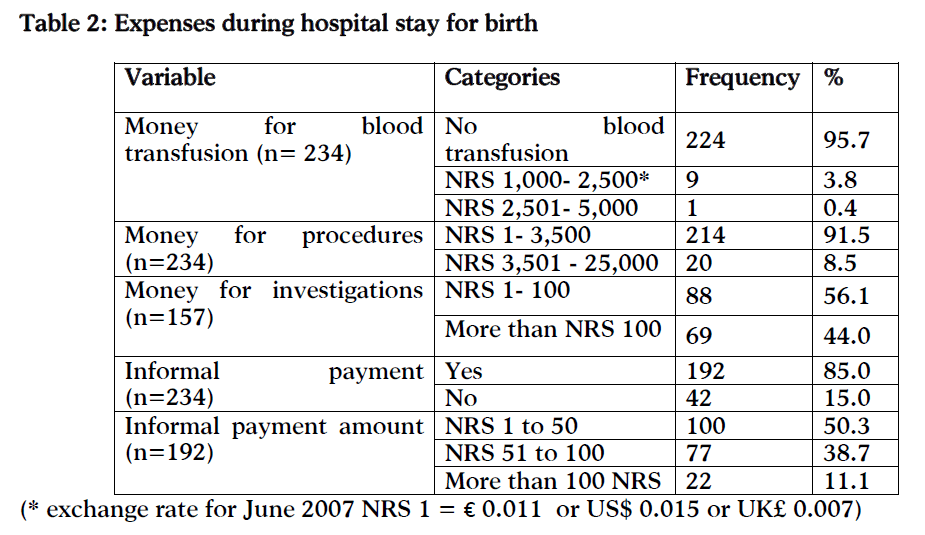
Most pregnancies were clinically uneventful, and only ten women required blood transfusion (Table 2). Only 9% of women spent more than NRS 3500 (€39.40) on drugs and procedures. The mean amount spent on hospital investigations was NRS 136 roughly equivalent to about 1½ Euro. The mean amount that a woman spent during her stay at the maternity hospital, including drugs, procedures and investigations was NRS 1,965 (€22.30). This excludes other informal payments. Table 2 indicates that 85% gave some sort of informal payments to ward attendants and ‘didis’ in the hospital. Almost half the respondents attested to giving payments up to NRS 50 (about 55 Euro cents), 33% paid between NRS 50 to NRS 100 and only 9% paid more than NRS 100 (€1.10).
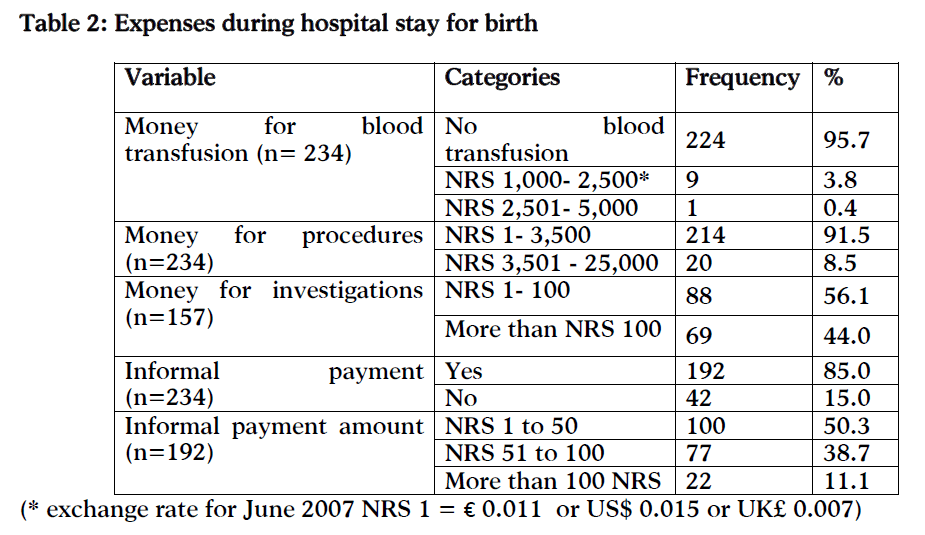
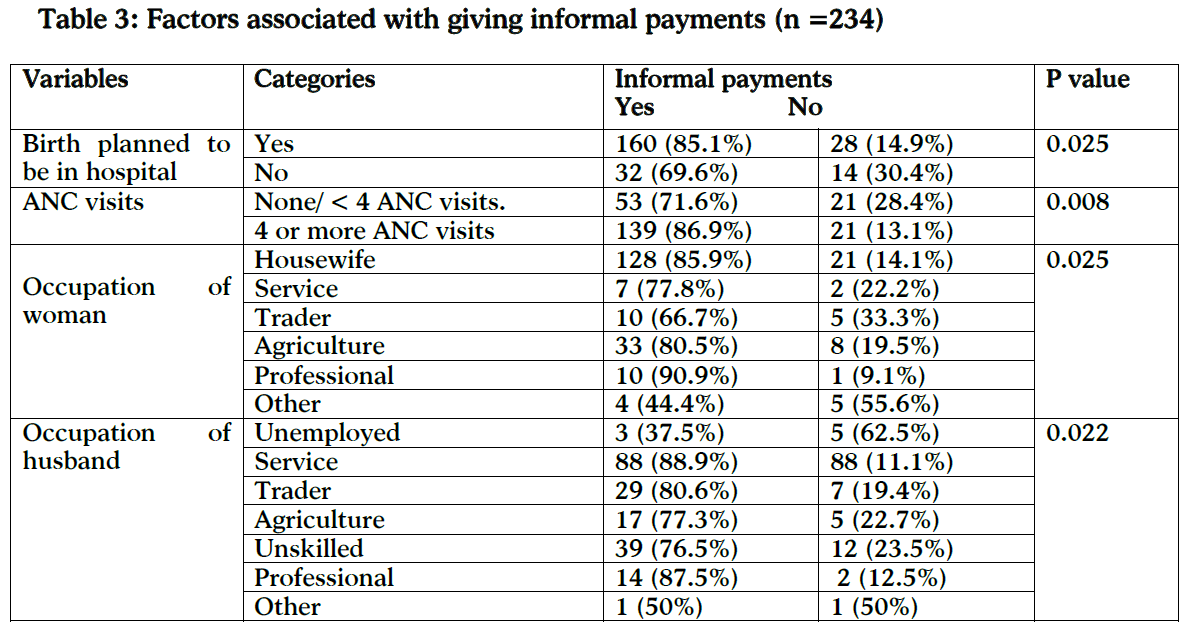
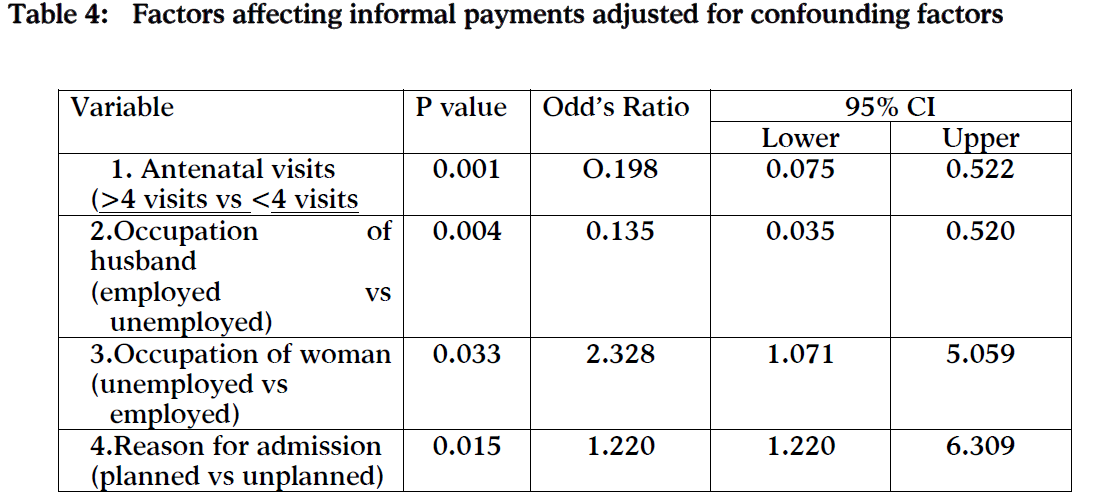
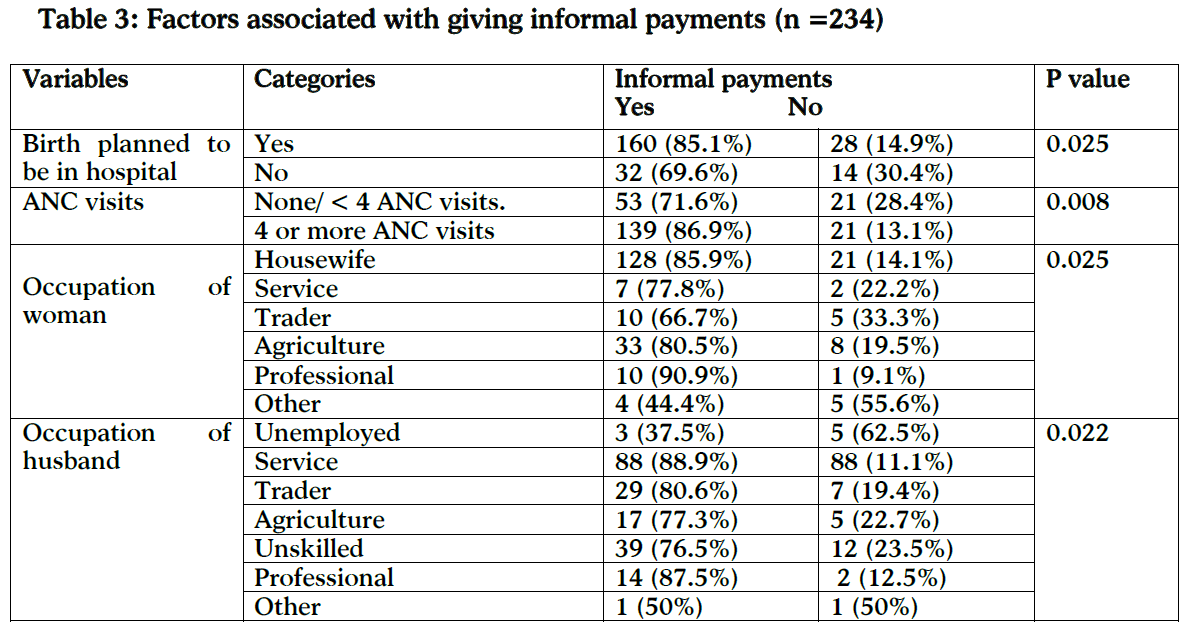
There was no significant association between making informal payments and the woman’s parity, p=0.807, woman’s age, p=0.437 her ethnicity, p=0.847, her educational status, p=0.533, family structure, p=0.442, her accommodation, p=0.615, monthly household income, p=0.210 or baby’s sex, p=0.567. Table 3 shows a significant association between making informal payments and whether or not the birth was planned to be in hospital or whether it was an emergency, p=0.025, ANC visits, p=0.008 woman’s occupation, p=0.025 and husband’s employment, p=0.022.
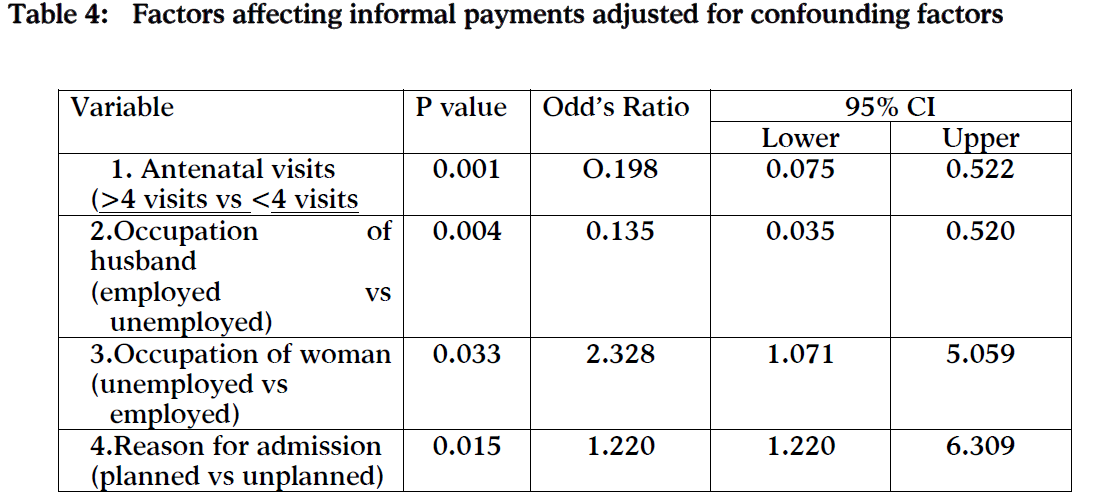
Binary Logistic Regression
After adjusting for the effects of the other significant factors identified above as well as possible confounders (residence, monthly household income or land ownership): (a) antenatal visits; (b) occupation of husband; (c), occupation of woman; and (d) reason for admission to hospital were all still significantly associated with the odds of making informal payments, p=0.001, p=0.004, p=0.033, p= 0.015 respectively. (Table 4).
Qualitative Results
Most interviewees had made savings’ arrangements prior to coming to the hospitals, husbands had taken up additional jobs, worked extra time or borrowed money from friends or family, and people depended heavily on their savings. In order to maintain anonymity only parity and age are provided with each quote.
A 23-year-old first-time mother said: “I left my job after I got pregnant but my husband is still working. We had some money saved that we (used) to pay the hospital bills.”
Some had problems arranging funds in time. For example, the 24-year-old husband whose wife needed an emergency caesarean section said: “She was admitted in the emergency and I was called by the doctor. He said … they needed to operate. They gave me a long list of medicines to buy and also told me to arrange blood. I did not have that much money but the medicine shop let me buy them on credit. I am trying to arrange some money to pay off the bills.”
The total cost associated with hospital stay varied from NRS 1,200–20,000 (ranging from €13.40 to €223.10) depending on the length of stay and whether there were complications.
The husband of a 24 year old multi gravida said, “We have been saving money for the delivery at the hospital. The hospital charges are reasonable. There are good doctors working here. It is the best government hospital and they also provide us food.”
All interviewees made informal payments to low-level hospital staff, mostly to ‘didis’ who work in the wards as maintenance staff or transport patients. Demands for money usually began after the delivery. The amount demanded generally varied according to the perceived economic status of the patient and most demands were for cash and not in-kind gifts. It was also seen that, making voluntary payments in the spirit of celebration as ‘bakas’ to welcome the newborn is a customary practice. Few interviewees had made informal payments for services rendered by the support staff such as washing garments, bathing the newborn or for helping out the women during her stay. Generally, payments were made either at the time of discharge, or demanded on the spot when services had been rendered. Prices were not fixed and bargaining was also common.
The husband of a 22-year-old first-time mother was hesitant when asked about any informal payments made: “We gave hundred rupees to the didi but it is nothing. I just gave it like that … because we are happy and she also gave the baby a bath.”
The latter quote suggests the family seemed to regard this more as a gratitude payment than a request for money from ward staff.
Discussion
Socio-demographic characteristics and utilization of maternity services
Our findings in terms of age of women (Table 1) are in line with national data, as the 2006 Nepal data show that the age distribution of mothers at birth is 17.7% below 20 years of age, 73.1% between 20- 34 and 9.2% over 35 years [5]. Hinduism is the major religion and a majority of our participants was Hindu. Contrary to the Nepalese norm [25], the majority of participants belonged to nuclear families. Increased costs of living in the capital coupled with the mass migration into the city due to recent conflicts are likely explanations for this difference.
Our study shows higher levels of education among women compared to other Nepalese studies [26], probably because (a) women with lower education and social status are more likelihood to deliver at home rather than in a hospital facility; and because the capital; (b) has better education facilities; and (c) a more enlightened attitude towards educating girls in recent years.
Nine out of ten women had at least one antenatal visit conducted by a skilled birth attendant, which is slightly higher than the national average of 85% [5]. Amongst these respondents 68.4% had received four or more antenatal visits.
Formal and informal user fees influence the utilisation of maternal health services, as was suggested in Laos [27] or India [28]. Opportunity costs of sickness and treatment is burdensome on poor people who depend on daily wages [29]. Direct fees as well as the cost of transportation, drugs and supplies, multiple demands on women’s time are major obstacles in the maternal health service utilisation in Nepal [14].
Spending money for ANC was sometimes seen as unnecessary where women do not experience any problems or illness during pregnancy, and therefore saw little direct benefit in attending ANC [30]. However our study suggests that the cost related delivery care is lower among women who had attended the recommended number of ANC, it may be their problem were recognised and dealt in early stage by not letting to develop serious condition. This eventually saved the cost involved in complication.
Women’s expenses related to their hospital stay
Most participants paid less than about €40 for delivery at the maternity hospital, the average monthly salary for a low-level government employee. The average amount that a woman spent during her entire hospital stay (including drugs, procedures and investigations) was NRS 1,965 (€22.30). A willingness-to-pay study showed that the average cost to a household of an institutional delivery for a normal delivery was 678 NRS (approximately €7.50) significantly lower than our findings [31]. This difference may have occurred because our study was conducted in Kathmandu and we included normal as well as the more expensive complicated deliveries. However, Borghi and colleagues also highlighted that when additional charges, opportunity and transport costs are added, the total amount paid exceeded 5,300 (approximately (€30) [10]. For example, for a caesarean section the total household cost was more than 11,400 NRS (approximately €60). Our findings are similar to a recent study of a similarly large government hospital in Bangladesh [19]. It is seen that the situation is exacerbated for complicated deliveries which usually cost households between three and ten times more than normal deliveries [21]. The cost of complicated deliveries is often catastrophic, i.e. in excess of 10% of yearly household income [32]. Poverty is closely link to women’s health needs and ability to use the services. Poor women are less able to afford skilled care at delivery [10]. Unlike the situation at the Maternity Hospital in Nepal, studies from other developing countries have also reported that in addition to the above mentioned payments, women also have to purchase supplies such as bleach to sterilise materials, bed sheets, gauze, gloves, and sanitary pads when admitted to a health facility for delivery [15,33]. In addition to costs related to maternity care there are also costs associated with food and living expenses [10,31]. Previous research from Nepal has shown that transport costs to a delivery facility are almost half of total delivery expenditure. Total (travel and waiting) time costs were estimated at 9 to 14% of total household expenditure for a delivery in Nepal [31].
Informal payments
Most gave an informal payment to the ward attendants and ‘didis’in hospital. These informal payments are flexible and generally demanded according to the perceived economic status of the patient. Our logistic regression found four factors associated with making informal payments: (1) planned hospital birth; (b) having attended four or more ANC sessions; (3) being a housewife; and (d) having a husband in paid employment. But we did not find any relation between the baby’s sex and the amount of money given, unlike a similar Indian study which suggested that the birth of a boy commanded a bigger “gift” [34].
Informal payments are deeply embedded in culture of health care in low-income countries. Killingsworth et al., [20] described a satellite system or a complementary market for non-medical services among the ward boys and ayahs who make beds and clean corridors in Bangladesh offering a range of additional ‘hotel’ services such as better food and offer collection of drugs from the market. Our qualitative data suggest that most couples had attempted to make financial arrangements prior to coming to the hospital through savings, but not all families had (or could) save money for this reason. Families had to borrow money to help pay the cost of delivery and/or depend on credit from supplies, such as pharmacists outside the hospital. For example, urban women attending the main government hospital in the capital of Bangladesh also were likely to borrow from neighbours and family [19].
The culture of corruption is endemic in most developing countries including Nepal, and affects all sectors of society. In 2008 Nepal ranked a dismal 121th out of 180 countries, according to Transparency International’s Corruption Perception Index [35]. Nepal is also in the bottom 25% on five of the World Bank’s six governance indicators due to its political instability and government ineffectiveness.
This study is one of the first of its kind in Nepal. The second strength is that it included a very large proportion (around 90%) of all women who had given birth in the key government hospital in a consecutive period in 2007. One of the weaknesses is that the study was conducted in one hospital, be it the largest government maternity unit in Nepal. However, we need to bear in mind that in Nepal 81% of births take place at home, many without skilled attendants [5]. On a more technical level, we had to estimate our response rate as it was not possible to establish the exact number of women who gave birth during our study period. Despite being in the hospital everyday a few women gave birth and left before the researcher could approach them about the study. The final weakness is that we only asked about costs that occurred in hospital which excludes transports cost to the facility.
Conclusions
Women have to pay for hospital delivery in urban Nepal, not just the formal registration fee, but also additional formal and informal costs. Total expenditure is significant for an average Nepalese household and more so for the poor.
Although informal payments around birth were not substantial, our study shows such payments are very common. Better understanding of informal payments is important as the illegal or quasi-legal status of unofficial health care payments means that it is very difficult to establish the prevalence of this phenomenon, but at the same time it forms a part of the private health expenditure rarely included in the national health statistics, they create perverse incentives, potentially reduce motivation for reform and will provide information about economic barriers to care.
In 2005 Nepal introduced the Safe Delivery Incentives Programme (SDIP) to promote the use of SBAs in public. These financial incentives are based on a cost sharing policy to promote SBAs and include conditional cash transfer and pay the woman for her travel to a health facility. Such incentives can contribute to greater equity in health care by making delivery services affordable, with subsidised prices for essential obstetric services or, better, free of charged.
Authors' contributions
All authors formulated the original idea for this paper. GS carried out the data collection and analysis for this study as a part of his M.Sc. research project at the University of Aberdeen, Scotland, UK. EvT and PS were supervisors of this public health research project and participated at all stages of the study and provided comments and suggestions on multiple drafts of this manuscript. BS provided considerable background reading and comments on drafts. JT was involved in the statistical analysis. All authors have read and approved the final manuscript.
Acknowledgements
The researchers would like to thank, first and foremost, all the women and their families who participated in this study and Dr Kasturi Malla, Former Director of the Prasuti Griha Hospital, Kathmandu who made it possible to conduct this research in Kathmandu. We thank Dr. Emma Pitchforth, LSE (UK) for providing us with useful references. We would also like to thank the Small Grants committee at the University of Aberdeen for providing financial support.
3243
References
- Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010; published online April 12. doi:10.1016/S0140-6736(10)60518-1.
- World Health Organization. Making pregnancy safer. Annual Report 2007. World Health Organization, Geneva, 2008.
- World Bank. Gross national income per capita 2008, Atlas method and PPP, 2009. online: https://siteresources.worldbank.org/DATASTATISTICS/Resources/GNIPC.pdf (accessed May 2010).
- World Bank. Data: Nepal 2010. Available on https://data.worldbank.org/country/nepal accessed on 29/11/10
- DHS. Nepal demographic and Health Survey 2006. Ministry of Health and Population Government of Nepal, New ERA Kathmandu Nepal and Macro International Inc. U.S.A., 2007.
- Sudevi BK, Pradhan A, Barnett S, Puri M, Chitrakar SR, Poudel P., et al. Nepal maternal Mortality and Morbidity Study 2008-2009: Summary of Preliminary Findings. Kathmandu, Nepal. Family Health Division, Department of Health Services, Ministry of Health, Government of Nepal, 2009.
- Furuta M, Salway S.: Women's position within the household as a determinant of maternal health care use in Nepal. International Family Planning Perspectives 2006;(1): 17-27.
- Shakya K., McMurray C. Neonatal Mortality and Maternal Health Care in Nepal: searching for patterns of association. Journal of Biosocial Science. 2001;33 : 87-105.
- DoHS and MoHP. National Safe Motherhood and Newborn Health Long Term Plan (2006-2017). Family Health Division, DoHS, Government of Nepal and Ministry of Health and Population 2009. Available in https://www.safemotherhood.org.np/pages/default.php?function=more_content&secid=74&con_id=44 Accessed : 28/09/10.
- Borghi J, Ensor T, Somanathan A, Lissner C, Mills A. Lancet Maternal Survival Series steering group. Mobilising financial resources for maternal health. Lancet. 2006; 368:1457–1465.
- Quayyum Z, Nadjib M, Ensor T, Sucahya PK. Expenditure on obstetric care and the protective effect of insurance on the poor: lessons from two Indonesian districts, Health Pol Plann. 2010; 25: 237–247
- SEARO/ WHO. Nepal Country Health System Profile: Trends in socio-economic development, 2007. Available in https://www.searo.who.int/en/Section313/Section1523_6863.htm Accessed: 24/11/10
- Powell-Jackson T, Wolfe R. Encouraging women to use professional care at childbirth, Does Nepal’s Safe Delivery Incentive Programme work? Evidence from the district of Makwanpur, 2008. Available in https://www.towards4and5.org.uk/PDFs/Nepal%20briefing%20note.pdf Accessed on 24/11/10
- Sharma B. Utilisation of Antenatal Care Services in Nepal. Nepal Pop J. 2004; 11: 79-97.
- Borghi J, Hanson K, Acquah CA, Ekanmian G, Filippi V, Ronsmans C, et al. Costs of near-miss obstetric complications for women and their families in Benin and Ghana, Health Pol Plann. 2003; 18: 383–392.
- Lee K. The Financing and Management of Primary Health Services, Asian Pac J Public Health. 1998; 2(2): 138-143.
- Perkins M, Brazier E, Themmen E, Bassane B, Diallo D, Mutunga A, Mwakajonga T, Ngobola O. Out-of-Pocket cost for facility-based maternity care in three African countries. Health Pol Plann. 2009; 24: 289-300.
- Balabanova D, McKee M. Understanding informal payments for health care: The example of Bulgaria. Health Pol. 2002; 62: 243–273.
- Pitchforth E, van Teijlingen E, Graham W, Dixon-Woods M, Chowdhury M. Getting women to hospital is not enough: a qualitative study of access to emergency obstetric care in Bangladesh Qual Saf Health Care. 2006;15: 214-219.
- Killingsworth J, Hossain N, Hedrick-Wong Y, Thomas SD, Rahman A, Begum T. Unofficial fees in Bangladesh: Price, equity and institutional issues. Health Pol Plann. 1999; 14:152-163.
- Green J. Qualitative Methods for Heath Research. London: Sage Publications, 2004.
- Forrest Keenan K, Teijlingen van ER. The quality of qualitative research in family planning and reproductive health care, J Fam Plann Reprod Health Care. 2004; 30(4): 257-59.
- Teijlingen van ER, Hundley V. The importance of pilot studies. Social Research Update 2001; 35. Online: https://sru.soc.surrey.ac.uk/SRU35.html/ Accessed: 1/4/ 2010.
- Forrest Keenan K, Teijlingen van ER, Pitchforth E. The analysis of qualitative research data in family planning and reproductive health care. J Fam Plann Reprod Health Care. 2005; 31: 40-43.
- Gilbert K. Women and Family Law in Modern Nepal: Statutory Rights and Social Implications. NY Univ J Int Law Pol. 1992; 24:729-758.
- Sreeramareddy CT, Joshi HS, Sreekumaran BV, Giri S, Chuni N. Home delivery and newborn care practices among urban women in western Nepal: a questionnaire survey. BMC Pregnancy Childbirth. 2006; 6: 27.
- Phoxay C, Okumura J, Nakamura Y, Wakai S. Influence of Women's Knowledge on Maternal Health Care Utilization in Southern Laos Asia Pac J Public Health. 2001; 13: 13-19.
- Griffith P, Stephenson R. Understanding users' perspectives of barriers to maternal health care use in Maharashtra, India. J Biosocial Sci. 2001; 33:339-359.
- World Bank. How do we Improve Maternal Health Outcomes? World Bank, 2009. Online: https://go.worldbank.org/20VS5LC7F0 Accessed: 1/2/2010.
- Simkhada BD, van Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilisation of antenatal care in developing countries: systematic review of the literature. J Advanc Nurs. 2008; 61: 244-260.
- Borghi J, Ensor T, Neupane B, Tiwari S. Financial implications of skilled attendance at delivery: the case of Nepal, Trop Med Int Health. 2006; 11: 228-237.
- Ranson K. Reduction of catastrophic health care expenditures by a community-based health insurance scheme in Gujurat, India: current experiences and challenges, Bull World Health Organ. 2002; 80: 613–621.
- Kowalewski M, Mujinja P, Jahn A. Can mothers afford maternal health care costs? User costs of maternity services in rural Tanzania, Afr J Reprod Health. 2002; 6: 65–73.
- Sharma S, Smith S, Sonneveldt E, Pine M, Dayaratna V, Sanders R. Formal and Informal Fees for Maternal Health Care Services in Five Countries: Policies, Practices and Perspectives (Policy Working Paper Series no. 16), USAID, 2005.
- Graf Lambsdorff J. Corruption Perspective Index. In: Global Corruption Report 2009, Transparency International UK, 2009. online: https://www.transparency.org/publications/gcr/gcr_2009#dnld. Accessed: 1/4/ 2010.