Keywords
Physical activity, behavioral and psychological correlates, Health Locus of Control, health related professionals, accelerometer
Introduction
The value of a physically active lifestyle as a means of protecting and promoting health is well recognized. It has been shown that physical activity (PA) decreases cardiovascular disease [1-3], averts or delays the development of high blood pressure [4,5], controls and prevents diabetes [6,7], normalizes weight [8], reduces the risk of osteoporosis [9,10] and forms of cancer [11], increases functional capability, improves depression and anxiety and contributes to a positive sense of well being [12,13]. In general a physically active way of life decreases the risk of mortality and increases longevity [14]. Unfortunately, people have not succeeded to understand the concept and health value of an active lifestyle [15].
A number of models and concepts that can possibly aid the understanding of PA participation have been discussed. The Locus of Control (LOC) model is one of them [16]. The first LOC scale was presented by Rotter (1966) [17] and was a measure of ‘individual differences in a generalized belief for internal or external control of reinforcement’. Since this scale was developed as a generalized measure, it was inevitable that researchers would develop more situation-specific measures of LOC to allow for better prediction of specific behaviors. One of the most widely used such measure is the Health Locus of Control (HLC) scale [18] designed for predicting health behaviors.
Dishman (1981) used the HLC scale to predict exercise adherence and drop-out in a 20-week prospective study of young adult men. They found that adherers had higher internal scores than drop-outs. Furthermore, subjects with external HLC were less likely to adhere to the programme than subjects with internal HLC. Moreover, Dishman and Steinhardt (1990) [20] studied the validity of HLC for predicting free-living PA among college students. They concluded that although HLC was unrelated to supervised PA, it could efficiently discriminate between high active and low active subjects. However, these studies did not use standardized assessments of PA. Therefore, their results cannot be easily generalized.
Another factor associated with PA participation is the knowledge of the benefits of PA21. However, studies implied inadequate counseling by health professionals [22,23]. Recommendations to improve physician counseling incorporate improving their personal PA habits, so that their guidance to patients can be more practical and effective [24]. These recommendations are reinforced by evidence that health professionals who are physically active themselves are more likely to counsel their patients about exercise [21].
Physiotherapists are among the health professionals that prescribe PA to their patients and a great proportion of their education consists of exercise training. However, little evidence exists with regard to the physiotherapist exercise counseling and its association with their activity levels and beliefs.
Research that wishes to address problems related to PA must be able to accurately quantify PA behavior [25]. Although a variety of techniques have been used to assess PA, none of these have been found to be both objective and practical [26].
The activPALTM, which combines the motion sensing approach with accelerometry, is a very small (35mm x 53mm x 7mm) and lightweight (20gr including battery) electronic device, designed to be worn on the mid-thigh. The activPALTM seems promising for use in PA research because it combines the advantages of accelerometry with the ability to register three classes of activity (sitting/lying, standing, stepping) second by second [27].
The present study aimed to provide evidence for the validity and reliability of the activPALTM and use it a) to identify any differences in the daily activity levels of physiotherapists and non-health related professionals and b) to test the validity of HLC scale as a predictor of PA levels.
Material and Methods
Validation of the activPALTM
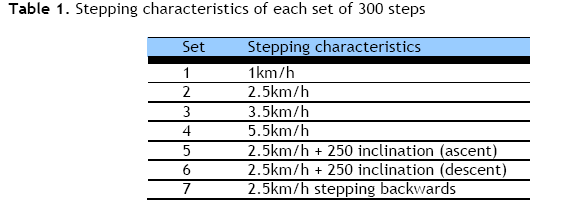
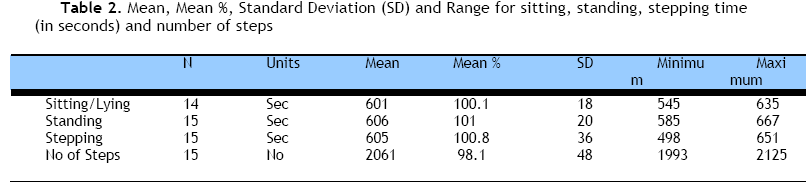
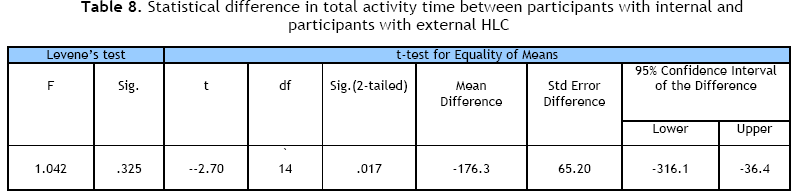
To evaluate the validity and test-retest reliability of the activPALTM a 28 years old female student repeated the same protocol of activities fifteen times. The protocol included two sessions. In session one the activities included 600 seconds sitting, 600 seconds standing and 600 seconds stepping [The activPALTM presents the recorded time in the format hours, minutes, seconds to proceed in further analysis the time of each activity was transformed in seconds]. In session two she performed seven sets of 300 steps each on a treadmill (total of 2100 steps). Each set had different stepping characteristics (Table 1). The activPALTM was placed on the participant’s right mid-thigh – midway between hip and knee. The percentage of the true value recorded for each output was calculated as 100 x device count / actual count. A value over 100 indicated over counting and a value under 100 indicated undercounting.
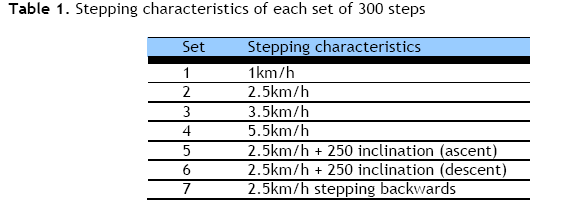
The activPALTM gave almost identical measures with the true values and the measures obtained showed little variation within the fifteen recordings (Table 2).
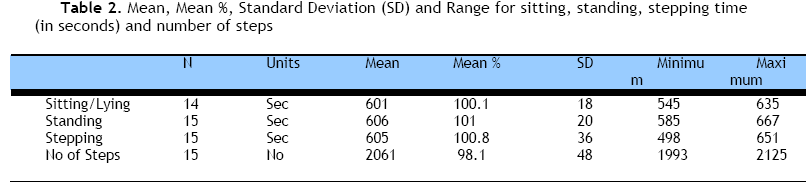
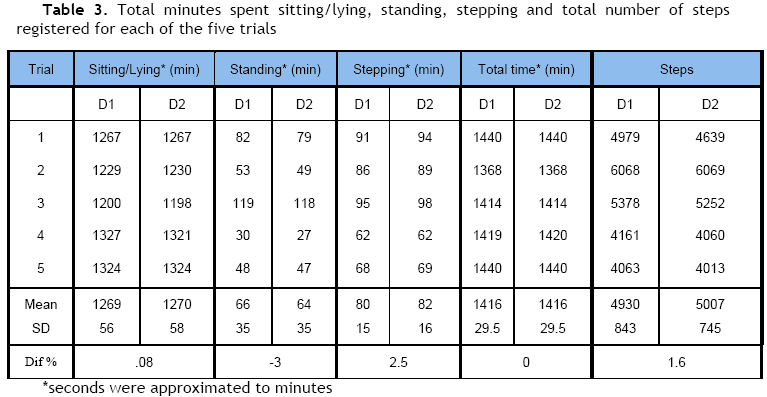
The inter-instrument reliability between the validated unit and a second that would be employed for further data collection was evaluated on the same participant. She had to wear both devices simultaneously on her right mid-thigh and be monitored for 24 hours. The 24 hours monitoring was repeated five times. Since the recording period was extensive, the time outputs were analysed in minutes. The mean difference in the output between the two devices 1 and 2 was calculated as 100 – (100 x mean Device 2 output/mean Device 1 output). Negative values indicated higher values in Device’s 1 output.
Device 2 measured .08% more sitting time, 3% less standing time, 2.5% more steps than Device 1(Table 3).
Operational definitions
Daily PA was defined as ‘the sum of the total standing time plus the total stepping time as measured by the activPALTM in a 24 hours interval’.
Design
An independent samples experimental design with two groups (physiotherapists and non-health related professionals) was used to examine how occupation affected HLC and daily PA.
Participants
A convenience sample of ten (10) physiotherapists and ten (10) non-health related professionals was used. All participants were recruited on voluntary basis. The participants were eligible to participate if they were between 22 and 32 and master’s level students pursuing a degree relevant to their occupation.
Ethics
Ethical approval was granted from the Queen Margaret University College’s, Edinburg, UK Ethics Sub-committee for the study’s procedure and the access to all participants.
Materials
The HLC Scale was used to measure HLC (Appendix I) [18]. The scale has been broadly employed in health behaviour studies and evidence of reliability and validity is summarized elsewhere [29].
The two validated activPALTM devices measured the daily PA of the participants.
Procedure
Eligible volunteers who consented to participate in the study completed the HLC Scale in a quiet room. Subsequently, the activPALTM, secured on the mid-thigh with Medipore tape, monitored their activities for 24 hours. Earlier the participants had been taught how to position it on their thigh, because they had to remove it during shower or bath. Each activPALTM was reprogrammed and a fresh battery was inserted in the device before each participant’s PA monitoring. The device was switched on and off by the researcher. Just after the participant had returned the activPALTM to the investigator, a few minutes semi-structure interview focusing on the participants’ views on the activPALTM was conducted (Appendix II). The interviews were taken and transcribed by the researcher in a quiet room.
Data Analysis
The HLC Scale was scored according to Wallston et al’s (1976) [18] instructions and was analyzed as a dichotomous variable (internal/external).
Since the activPALTM’s software displays only one day’s recording at a time, if a participant’s recording covered more than 24 hours (one day), the first recorded day was selected for further processing. The recorded time was analyzed in minutes.
The interview data were analyzed using the grounded theory [30]. Recurrent themes and emergent concepts were identified enabling the researcher to produce a framework that clarified the participants’ views on the activPALTM as a measurement of daily PA.
Results
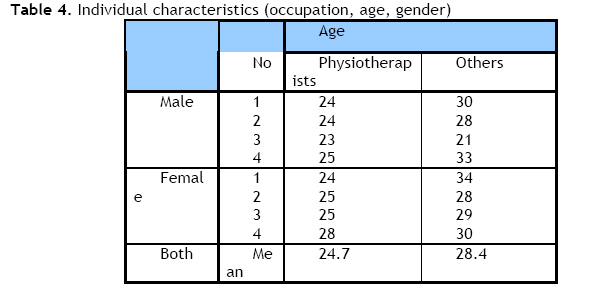
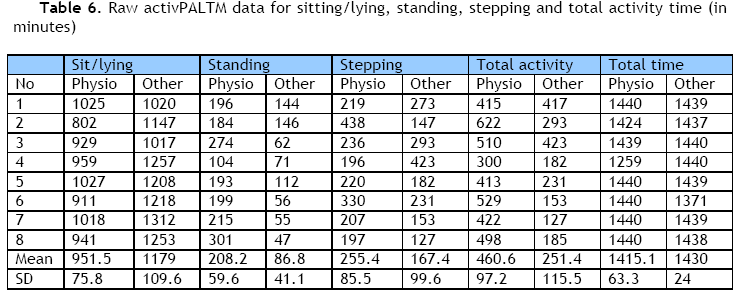
Twenty participants were tested. The activPALTM failed to give results in four occasions due to technical failure. Therefore, usable data were obtained for sixteen participants, eight physiotherapists and eight non-health related professionals (Table 4).
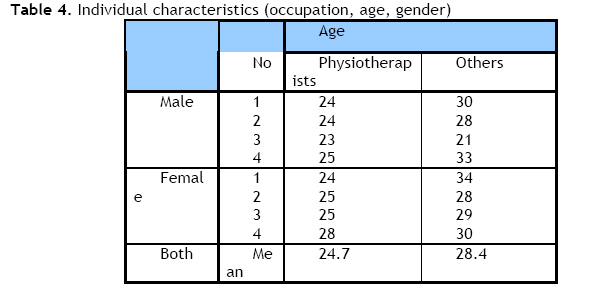
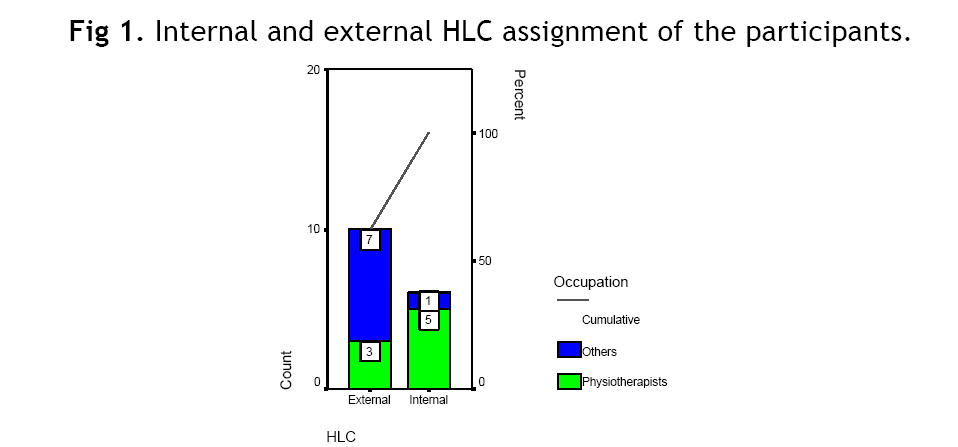
Figure 1 presents how the participants were assigned to external and internal HLC.
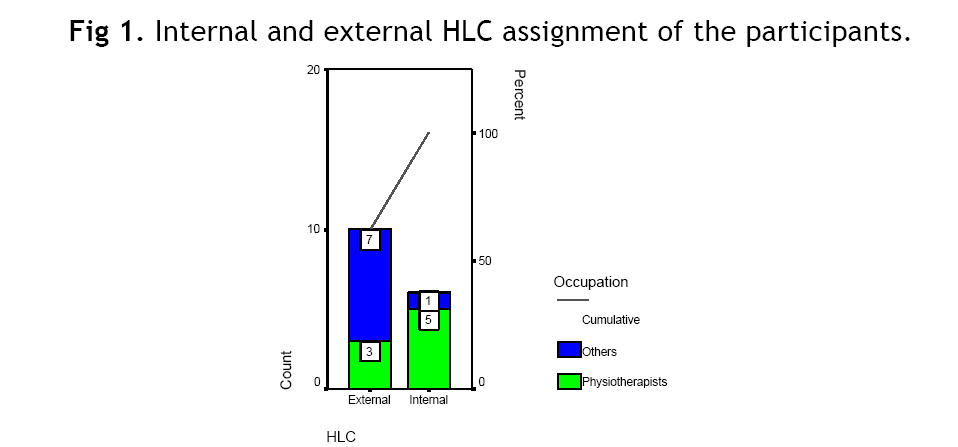
Figure 1: Internal and external HLC assignment of the participants.
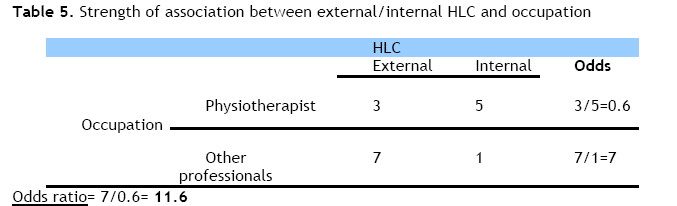
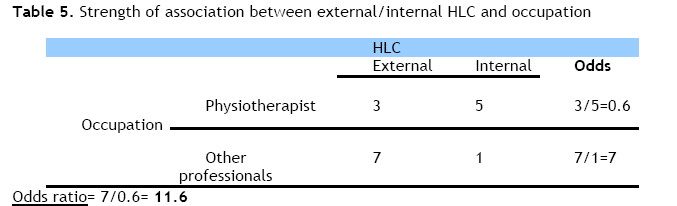
In order to identify the strength of association between the two dichotomous variables (occupation and internal/external HLC) the odds and the odds ratio were used. The odds is a measurement typically used for binary data, equal to the ratio of the probability of a event occurring divided by the probability of an event not occurring. The odds ratio is a ratio between two odds, used to summarize the strength of the relationship between two usually dichotomous variables. The odds and the odds ratio take values from 0 to infinity with 1 indicating indifference or lack of relationship [31]. The odds ratio suggested that the odds of having an external HLC were 11.6 times as high among non-health related professionals as among physiotherapists (Table 5).
Raw data and summary statistics for the time spent in each activity by the two groups are given in the Table 6. The recorded time for the two groups was the same. Stepping and standing time were added together to give total activity time (defined as daily PA).
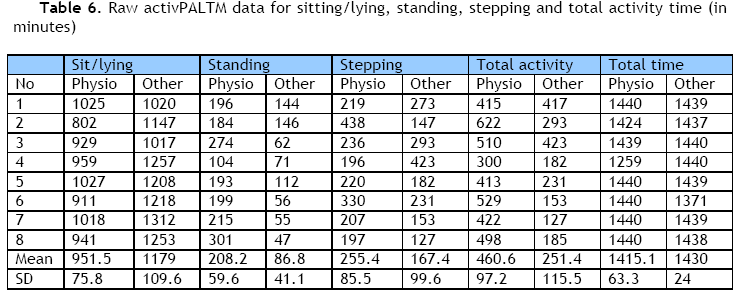
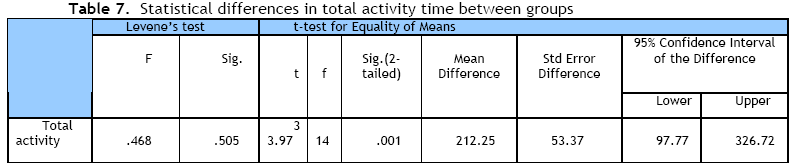
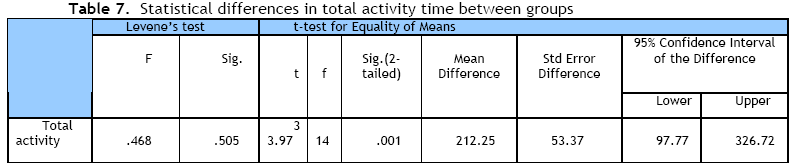
An independent-samples t-test was conducted to compare the total activity times for physiotherapists and non-health related professionals since the data satisfied the parametric assumptions. The results indicated significant difference in total activity time between physiotherapists (M=463.6, SD=97.1) and non-health related professionals [M=251.4, SD=115.5, t (14) =3.97, p=0,001] (Table 7). The magnitude of the differences in the means was large (eta squared=0.53) (Cohen 1988).
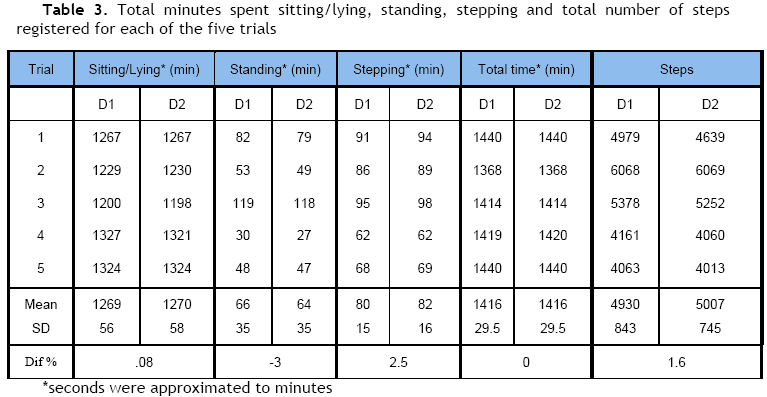
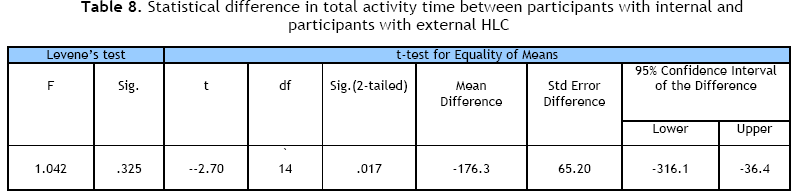
An independent samples t-test was used to compare the total activity times for internals and externals. The results with equal variance assumed indicated that the participants with external HLC (M=291.4, SD=134) had statistically significant lower total activity time compared with participants with internal HLC [M=467.66, SD=110.9c, t (14) =-2.70, p<0,05] (Table 8). The magnitude of the difference in the means was large (eta squared=.34).
Interview data
The participants regarded the activPALTM a valid and practical measurement of PA because it provides minute-to-minute monitoring of the main expression of PA and at the same time it is manageable, unobtrusive and fits easily under clothing. However, they mentioned that it would not reflect accurately the activity levels of populations that perform water activities or are in a wheelchair because it is not waterproof and does not detect activities of the upper body.
Discussion
The results support that physiotherapists are significantly more active than the non-health related professionals. Physiotherapists are comprehensively educated about PA benefits. Hence, the present study supports the findings of Clever and Arsham (1984) [24] who associated the knowledge of PA health benefits with the PA levels.
The examination of the physiotherapists PA behavior was prompted by evidence that health professionals can have a positive effect in their patient’s health behavior through counseling [32]. Effective PA counseling depends on health professionals’ personal activity habits [33] because health professionals who are physically active themselves are more likely to counsel their patients about exercise and give more effective PA guidance [21]. Our results imply that physiotherapists have recognized the importance of PA. However, the hypothesis that physiotherapists with high PA levels tend to counsel more about PA is yet to be examined.
The results also indicated that participants with internal HLC were statistically significant more active than participants with external HLC. Between the two groups tested, the most active group (physiotherapists) presented mostly internal HLC. The less active group (non-health related professionals) presented mostly external HLC.
Previous studies on the association of HLC with PA have resulted in contradictory evidence. O’Connel and Price (1982) [34] suggested that participants that adhere to exercise programmes are slightly more internal than drop-outs. In contrast, Laffrey and Isenberg (1983) [35,36] found no relationship between internal HLC and PA practices. Finally, Dishman and Steinhardt (1990) [20] supported the validity of HLC in predicting free-living PA among college students.
The results of the present study cannot be easily generalized. Firstly, the PA of the participants was monitored only for 24 hours. The results might be indicative but it is not certain that habitual PA activity is represented. Secondly, physiotherapists in general are familiar with the HLC theory and the value of PA to health. This fact may have influenced the findings that address the association of PA levels with HLC scores. However, the strong relationship between internal/external HLC and free-living PA that was identified justify experimental studies to examine the associations of HLC with PA in different populations.
Activity monitors have been extensively used in PA research because they are generally easy to administer and score and are acceptable to participants. Moreover, by continuous minute-to-minute monitoring of daily physical activity, they offer an objective alternative to self-report instruments typically used in this area of work. However, it has been shown that they underestimate activity time and number of steps up to 20% [37,38], overestimate time spent in sedentary activities [39] and have large variability within their recordings [40].
The activPALTM seems a promising alternative to previously used activity monitors. It gave almost identical measured and true values for sitting/lying, standing and stepping time and number of steps. The repeatability of the values obtained was high and recordings from two different activPALTM devices were highly correlated with each other. Speed, a factor that influences the recordings of most activity monitors [26,39] does not seem to affect the activPALTM recordings. Finally, the participants’ regarded the activPALTM as a practical and valid measurement of PA. This preliminary evidence suggest that the activPALTM is a useful PA measurement and justifies further research to establish its validity in different settings and populations and to test the accuracy of the step frequency and energy expenditure outputs.
Conclusion
The present study suggested that physiotherapists are more active and have a more internal Health Locus of Control than non-health related professionals, probably due to their education. The strong association of HLC with PA levels found implies that HLC model may have large potential in explaining free-living PA. However, studies are needed to confirm these results in different populations.
The PA of our participants was measured with the activPALTM activity monitor which was found valid and reliable in evaluating PA in populations that the majority of PA consists of ambulation. It could be valuable not only in measuring degree of physical activity of healthy individuals, but also in estimating activity of individuals undergoing rehabilitation interventions to improve ambulation and physical activity.
Acknowledgements
The authors want to thank Dr. Douglas Maxwell, Glasgow University, Glasgow, for his immediate response when he was asked for technical support and the QMUC postgraduate students that kindly participated in this study.
3645
References
- Paffenbarger RS, Jr., Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med 1986; 314:605-613
- Leon AS, Connett J, Jacobs DR, Jr., Rauramaa R. Leisure-time physical activity levels and risk of coronary heart disease and death. The Multiple Risk Factor Intervention Trial. Jama 1987; 258:2388-2395
- Morris JN, Clayton DG, Everitt MG, Semmence AM, Burgess EH. Exercise in leisure time: coronary attack and death rates. Br Heart J 1990; 63:325-334
- Roman O, Camuzzi AL, Villalon E, Klenner C. Physical training program in arterial hypertension. A long-term prospective follow-up. Cardiology 1981; 67:230-243
- Blair SN, Goodyear NN, Gibbons LW, Cooper KH. Physical fitness and incidence of hypertension in healthy normotensive men and women. Jama 1984; 252:487-490
- Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS, Jr. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N Engl J Med 1991; 325:147-152
- Manson JE, Nathan DM, Krolewski AS, Stampfer MJ, Willett WC, Hennekens CH. A prospective study of exercise and incidence of diabetes among US male physicians. Jama 1992; 268:63-67
- Yamanouchi K, Shinozaki T, Chikada K, Nishikawa T, Ito K, Shimizu S, et al. Daily walking combined with diet therapy is a useful means for obese NIDDM patients not only to reduce body weight but also to improve insulin sensitivity. Diabetes Care 1995; 18:775-778
- Dalsky GP, Stocke KS, Ehsani AA, Slatopolsky E, Lee WC, Birge SJ, Jr. Weight-bearing exercise training and lumbar bone mineral content in postmenopausal women. Ann Intern Med 1988; 108:824-828
- Marcus R, Drinkwater B, Dalsky G, Dufek J, Raab D, Slemenda C, et al. Osteoporosis and exercise in women. Med Sci Sports Exerc 1992; 24:S301-307
- Lee IM, Paffenbarger RS, Jr., Hsieh C. Physical activity and risk of developing colorectal cancer among college alumni. J Natl Cancer Inst 1991; 83:1324-1329
- Ross CE, Hayes D. Exercise and psychologic well-being in the community. Am J Epidemiol 1988; 127:762-771
- Stephens T, Craig CL. The well-being of Canadians: highlights of the 1988 Campbell's survey. Canadian Fitness and Lifestyle. Ottawa, 1990
- Blair SN. 1993 C.H. McCloy Research Lecture: physical activity, physical fitness, and health. Res Q Exerc Sport 1993; 64:365-376
- Duppert PM. Exercise in behavioural medicine. Journal of Consulting and Clinical Psychology 1992; 60:613-618
- King AC, Blair SN, Bild DE, Dishman RK, Dubbert PM, Marcus BH, et al. Determinants of physical activity and interventions in adults. Med Sci Sports Exerc 1992; 24:S221-236
- Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr 1966; 80:1-28
- Wallston BS, Wallston KA, Kaplan GD, Maides SA. Development and validation of the health locus of control (HLC) scale. J Consult Clin Psychol 1976; 44:580-585
- Dishman RK. Biologic influences on exercise adherence. Res Q Exerc Sport 1981; 52:143-159
- Dishman RK, Steinhardt M. Health locus of control predicts free-living, but not supervised, physical activity: a test of exercise-specific control and outcome-expectancy hypotheses. Res Q Exerc Sport 1990; 61:383-394
- Abramson S, Stein J, Schaufele M, Frates E, Rogan S. Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med 2000; 10:40-48
- Wells KB, Ware JE, Jr., Lewis CE. Physicians' practices in counseling patients about health habits. Med Care 1984; 22:240-246
- Orleans CT, George LK, Houpt JL, Brodie KH. Health promotion in primary care: a survey of U.S. family practitioners. Prev Med 1985; 14:636-647
- Clever LH, Arsham GM. Physicians' own health--some advice for the advisors. West J Med 1984; 141:846-854
- Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Jama 1995; 273:402-407
- Welk GJ. Physical activity assessments for health-related research. Human Kinetics. Champaign, 2002
- Barbenel JC, Maxwell DJ. MTS Project AM1: Development of lifetime prediction test methods for orthopaedic implant. Development of reference loading spectrum: I-Description of Daily Activities. Bioengineering Unit: University of Strathclyde, Glasgow, 1995
- Lau RP. Beliefs about control and health behavior. In: Gochman DS, ed. Health Behavior: Emerging research perspectives. New York: Plenum Press, 1988
- Wallston BD, Wallston KA. Locus of control and health: a review of the literature. Health Educ Monogr 1978; 6:107-117
- Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. London: Sage, 1990
- Howitt D, Cramer D. An introduction to statistics in psychology: a complete guide for students. 2nd ed. London: Prentice Hall, 2000
- Lewis CE, Clancy C, Leake B, Schwartz JS. The counseling practices of internists. Ann Intern Med 1991; 114:54-58
- Serman SE, Hershman WY. Exercise counselling: how do general internists do? J Gen Intern Med 1993; 8:243-248
- O'Connell JK, Price JH. Health locus of control of physical fitness-program participants. Percept Mot Skills 1982; 55:925-926
- Laffrey SC, Isenberg M. The relationship of internal locus of control, value placed on health, perceived importance of exercise, and participation in physical activity during leisure. Int J Nurs Stud 1983; 20:187-196
- Laffrey SC, Isenberg M. The relationship of internal locus of control, value placed on health, perceived importance of exercise, and participation in physical activity during leisure. International Journal of Nursing Studies (1983), 20, 187-196. Int J Nurs Stud 2003; 40:453-459; discussion 461-452
- Bassett DR, Jr., Ainsworth BE, Leggett SR, Mathien CA, Main JA, Hunter DC, et al. Accuracy of five electronic pedometers for measuring distance walked. Med Sci Sports Exerc 1996; 28:1071-1077
- van den Berg-Emons HJ, Bussmann JB, Balk AH, Stam HJ. Validity of ambulatory accelerometry to quantify physical activity in heart failure. Scand J Rehabil Med 2000; 32:187-192
- Nichols JF, Morgan CG, Sarkin JA, Sallis JF, Calfas KJ. Validity, reliability, and calibration of the Tritrac accelerometer as a measure of physical activity. Med Sci Sports Exerc 1999; 31:908-912
- Meijer GA, Westerterp KR, Verhoeven FM, Koper HB, ten Hoor F. Methods to assess physical activity with special reference to motion sensors and accelerometers. IEEE Trans Biomed Eng 1991; 38:221-229