Keywords
Healthcare systems; Cancer analysis
Introduction
Cancer has grown into one of the major causes of death in the world, especially in the higher income countries, where cancer is among the top causes of death [1]. The World Health Organization (WHO) estimates a growth of 50% in the number of cancer cases all over the world in the first two decades of the 21st century, achieving 15 million of new cases in 2020 [2]. Although mortality varies greatly between different cancers, 8.2 million people worldwide died from cancer in 2012 [3]. In Europe, this value is 29% (for men) and 23% (for women) [4]. Such numbers, along with the fact that cancer usually requires costly treatments, provide a special motivation for the present study.
Although European Union (EU) members have its own health-care system and each national government is the main responsible for its health-care funding and policies, EU has some community healthcare stipulations, as the right of access to preventive healthcare and medical treatment to everyone, [5] and has also been developing joint efforts to increase the quality of cancer-related health care.
Two of the main focuses of the actions taken by EU in cancer fight are efficiency and effectiveness, for the sharing that results from the aforementioned projects may contribute to avoid scattered actions and duplication of efforts, and the better usage of limited resources available [4,6,7]. Therefore, both indicators in health-care are main concerns in the EU project.
What is more, “achieving high value for patients must become the overarching goal of health care delivery, with value defined as the health outcomes achieved per dollar spent” [8]. Accordingly “value” is an interesting perspective for analyzing a health system, workflow or an institution. Such “value” is the reason why so many stakeholders have been summed around a system such as healthcare delivery. Literature has already plenty of published works regarding this matter. In this particular study, we will try to look beyond cancer survival and costs, by analyzing their ratio as a tool to measure efficiency. The objective of the present article is to understand which countries are showing better capabilities to give their citizens more chances of cancer survival, while spending just the necessary resources.
Literature Review
Effectiveness and efficiency come together when we analyze indicators of performance in health care, because them both add an economic dimension to health care [8]. Before measuring the system's efficiency, we must identify the actions that are effective. By effectiveness Madore, [8] defined it as “the relationship between the level of resources invested and the level of results, or improvements in health. Assessing effectiveness consists of measuring the effects of medical practices and techniques -- therapeutic, diagnostic, surgical and pharmacological -- on individuals' health and wellbeing.”
However, it is also necessary to bring along the perspective of costs. Moreover, the concept of efficiency needs to be put in the context of healthcare.
A working definition of efficiency is: “Efficiency is an attribute of performance that is measured by examining the relationship between a specific product of the health care system (also called an output) and the resources used to create that product (also called inputs)”[7]. Madore [8] also defined efficiency as “the relationship between the level of resources invested in the health care system and (…) improvements in health achieved”. In an attempt to rebuild from economic crisis, the relevance of achieving goals with reduced inputs has grown more than ever. The purpose of efficiency in healthcare European systems is to maximize outcomes effectively given a specific budget [8].
We can find many published studies about costs/resources invested and outcomes in cancer. We would like to highlight two of them. Firstly, Luengo-Fernandez et al. [9] report the economic costs of cancer, including the costs per person (adjusted by the purchasing-power parity) of the main types of cancer: colorectal, lung, breast and prostate cancer. They considered three different types of costs: health-care, informal care and productivity costs. Thoroughly, five categories of costs of care were considered: primary; outpatient; emergency; inpatient; and drugs. This data on costs will also be important for the proposed research in “value” since these studies, which are both systematic and vast, are scarce in literature. On the other hand, Angelis et al. [10] estimated the 5-year relative survival of skin melanoma, non-Hodgkin lymphoma and breast (women only), stomach, colon, rectal, lung, ovarian, prostate and kidney cancers. The results show, as expected, very different survival rates for different types of cancer. As far as these rates are concerned, economic wealth, sex and age are significant explanatory variables for the differences found across the countries, and there’s been a slight increase in these rates over the recent years.
Some studies go further and try to relate outcomes with resources used in health care. For instance, Ades et al. [11] tested the hypothesis that less national wealth implies increased cancer mortality, particularly in the case of diseases with effective treatments and screening methods, like breast cancer. The sample was divided in two population groups: Western and Eastern Europe. The first group consists of countries that have joined the EU before 1995 – the EU-15 countries. The second group considers the other 12 EU countries. Observing the mortality/incidence ratio and wealth indicators relation, it’s evident the existence of a negative and significant correlation between them. The reason for Western Europe’s incidence results may relate with unhealthy habits, while its relatively low mortality it’s probably attributable to early diagnosis.
Methodology
Recent research, as explained, focused on specific aspects (outcomes or costs, for example) that can be brought together in a logical manner. In fact, this article benefits from the outcomes of Luengo-Fernandez et al. [9] and from Angelis et al. [10] that provide important data with reliability and covering recent periods.
This research article aims at comparing value in the delivering of healthcare to cancer patients in several countries in Europe. In doing so, we operationalize Porter’s definition of value measurement where “the concept of value refers to the output achieved relative to the cost incurred” [12]. As a method, we used meta-analysis to innovatively combine some indicators from the aforementioned literature and we used Porter’s concepts on value in health care (VHC) in order to compare cancer health care across the Europe. The variables we’ve used were the 5-year age-standardized relative survival for adult patients [10], as an effectiveness measure, and the estimated cost per person by disease [9]. These variables were combined in a ratio between survival and adjusted costs per person, denominated as Value in Health-Care (VHC), that we use as a tool for measure efficiency.
In this research some assumptions were made. Firstly, some countries were excluded because they lacked the survival results (Cyprus, Greece, Hungary, Luxembourg and Romania) or the cancer-related costs (Croatia). Secondly, since Angelis et al. [10] provided information for each of UK’s countries separately and Luengo-Fernandez et al. [9] estimated adjusted costs per person for the UK as a whole, we assumed these UK’s costs as a standard for each of those countries. Thirdly, with respect to colorectal cancer, we calculated separate scores of VHC for colon and rectum, but assume the same colorectal cancer adjusted cost per person for both colon and rectal cancer.
Results
A different view on previously published data
Concerning the concept of effectiveness, we accomplish that survival results are better in Germany (DE), Austria (AT), Belgium (BE), Sweden (SW) and Finland (FI), while countries like Latvia (LV), Lithuania (LT), Bulgaria (BG) and Poland (PL) have usually lower results; survival rates differ considerably between diseases, but the ranking order of countries isn’t that different across all cancer types. Colon cancer survival oscillates between ≈62% in Germany and ≈43% in Latvia; in Bulgaria, Poland and Lithuania survival is also below 50%, and the results of Denmark (DK) and UK are also below the average, in spite of their position as the 20th and 21st countries in the world in GDP per capita (PPP) [13]. Rectal cancer presents a larger difference between the highest survival (Belgium, ≈63%) and the lowest (Latvia, ≈36%). Lung cancer is the most differentiated of all cancers: not only its survival is very low when compared to others, its mortality “tends to be primarily dependent on lifestyle or environmental factors rather than healthcare system performance” [15] what would probably help to explain that countries like Poland and Latvia present better rates than Finland, Portugal (PT) and Spain (ES).
As for the adjusted cost per person, Luengo-Fernandez et al. [9] show that Germany is clearly above all the other countries, followed by Netherlands (except for prostate cancer, which has Finland at second place). Austria also has high cancer-related costs per person, while Latvia, Lithuania and Bulgaria have the lowest cancer-related costs per person.
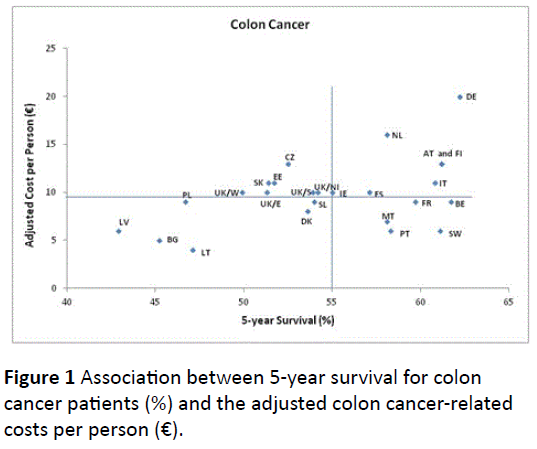
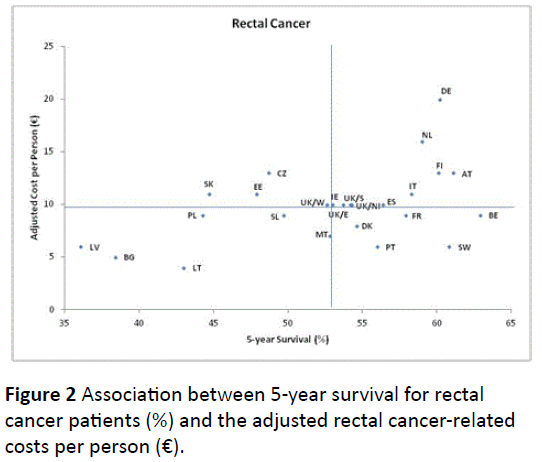
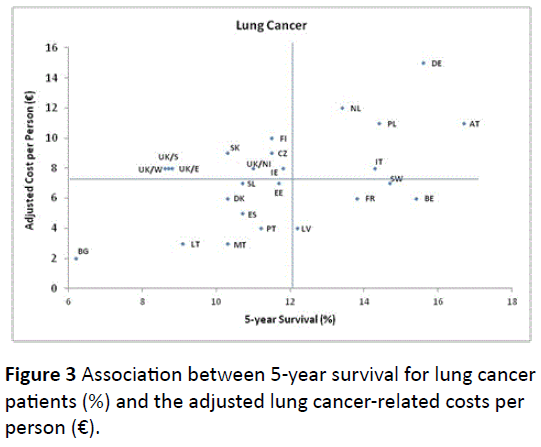
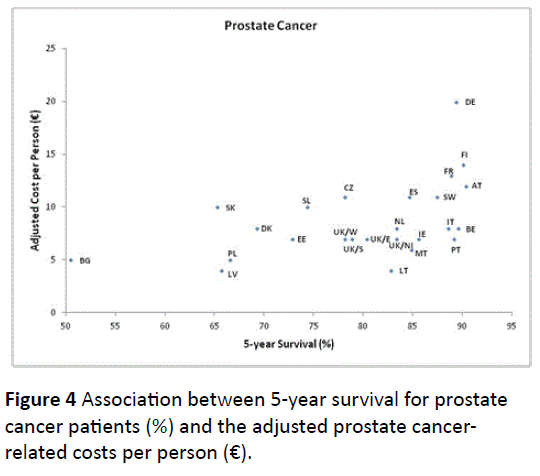
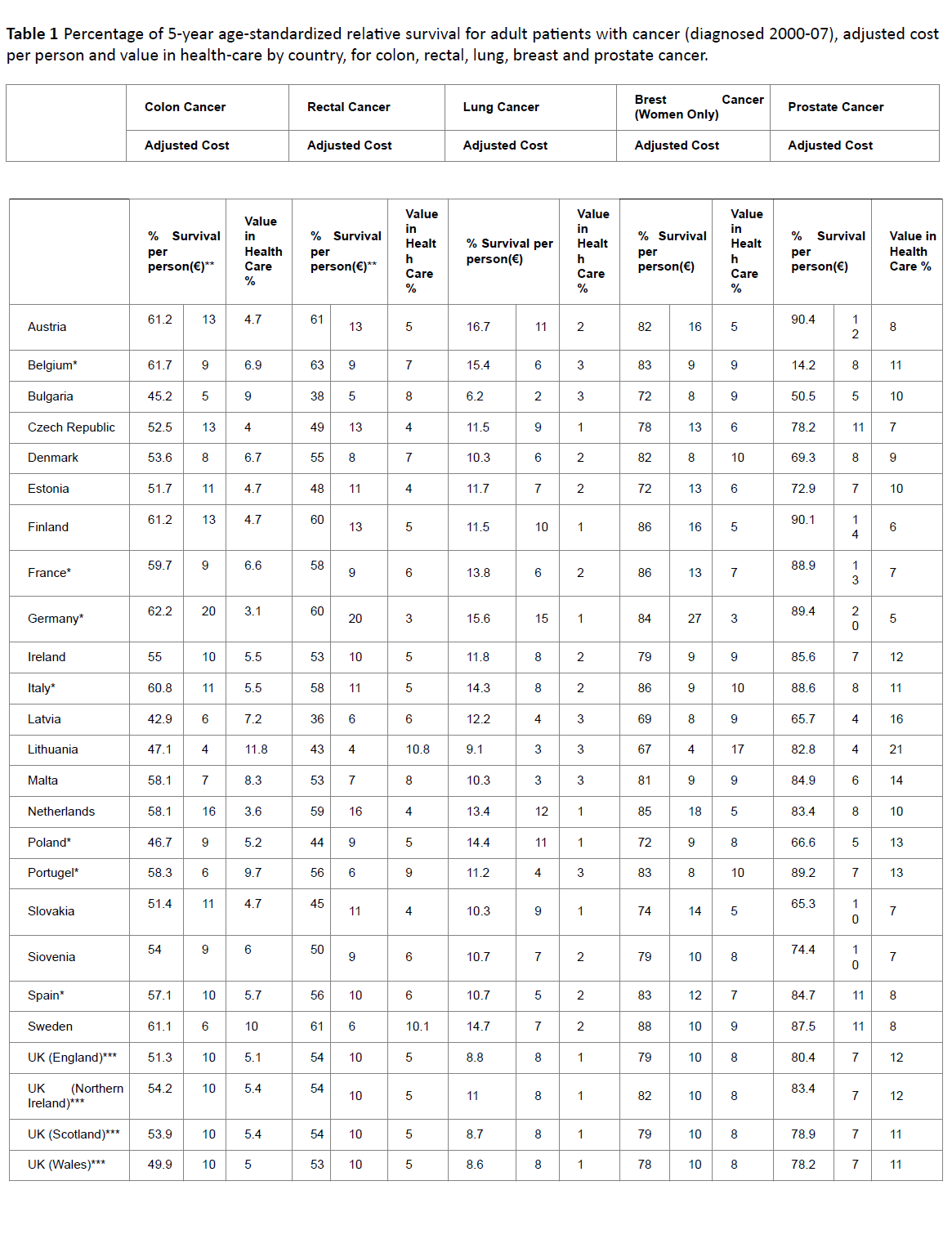
The following graphics relate survival and adjusted costs per person for each cancer, in an economic view they relate effectiveness with costs. The graphs represent the adjusted cost per person average (x-axis) and the 5-year survival average (y-axis), for the all countries. Counterclockwise, quadrant I represents countries in which both 5-year survival and adjusted cost per person is above the group’s average; in quadrant II are located countries with above-average adjusted costs per person but below the average in 5-year survival; countries where both indicators are below the average value are in quadrant III and countries with better results in 5-year survival with relatively low costs occupy quadrant IV.
For both colon and rectal cancers (Figures 1 and 2), Germany and at a lesser extent Netherlands (NL) stand out from the rest of the sample, in the top of quadrant I; they share this quadrant with Austria, Finland, Italy (IT) and Spain. The opposite quadrant is occupied by Latvia, Bulgaria and Lithuania, while Poland is closer to quadrant II. Belgium and Sweden are the countries of quadrant IV achieving higher survival, followed by France (FR) and Portugal. Denmark is also located in the quadrant IV of rectal cancer, but the colon cancer’s graph has this country in quadrant III. The Pearson correlation between these variables, for colon cancer, is slightly positive (r≈0.46) and significant (p-value≈0.019). Rectal cancer has similar results (r≈0.47, p-value≈0.017).
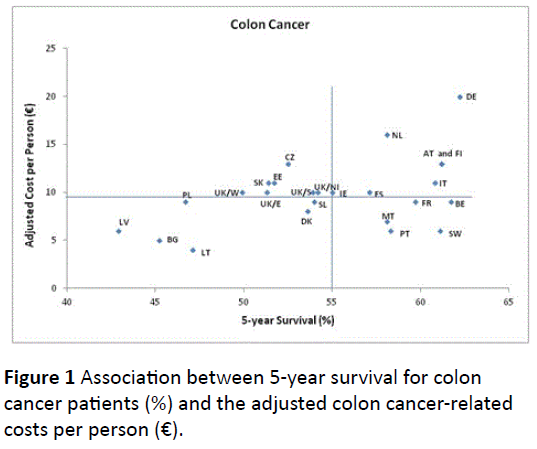
Figure 1: Association between 5-year survival for colon cancer patients (%) and the adjusted colon cancer-related costs per person (€).
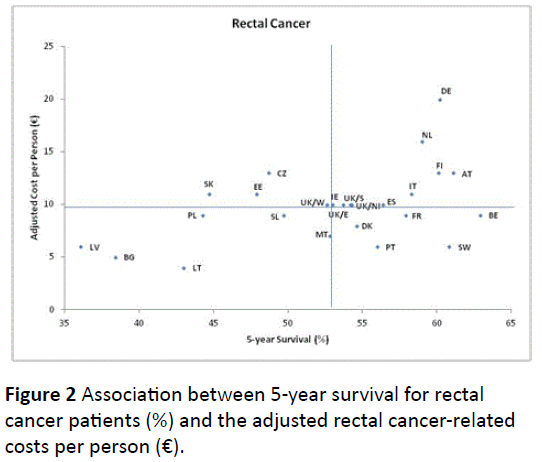
Figure 2: Association between 5-year survival for rectal cancer patients (%) and the adjusted rectal cancer-related costs per person (€).
For lung cancer (Figure 3), Belgium, Sweden, France and Latvia are achieving above-average survival results, while spending less. UK, Slovakia, Czech Republic (CZ), Finland and Ireland (IE) are having bigger expenditures than the average, yet registering a lower survival.
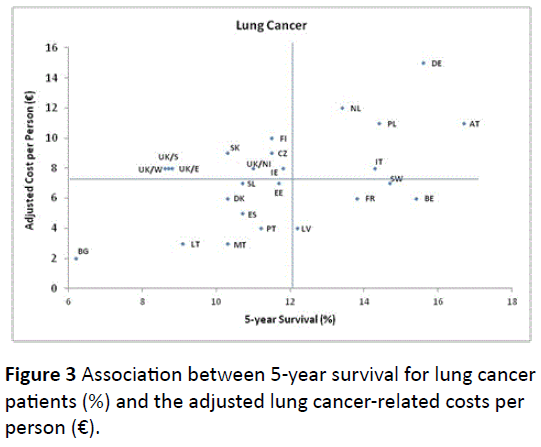
Figure 3: Association between 5-year survival for lung cancer patients (%) and the adjusted lung cancer-related costs per person (€).
Prostate cancer (Figure 4) has Belgium, Portugal and Italy as examples of countries that, despite having lowest expenditure per capita, still present good survival results. In the same quadrant stand Ireland, Malta (MT), Netherlands and Lithuania, with the UK is standing between quadrants IV and III. Austria, Finland, France, Sweden, Spain and especially Germany have high costs, while also achieving good survival levels.
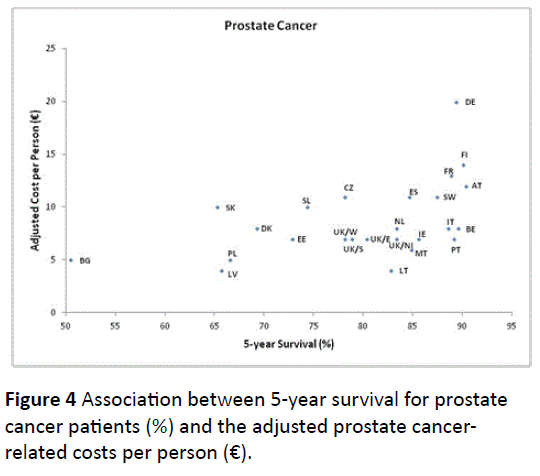
Figure 4: Association between 5-year survival for prostate cancer patients (%) and the adjusted prostate cancerrelated costs per person (€).
Quadrant I of the breast cancer graph (Figure 5) is very heterogeneous: Germany detaches from the others for its larger costs. Quadrant IV has Italy and Sweden on the top right side, with Portugal and Belgium as the closer followers.

Figure 5: Association between 5-year survival for breast cancer patients (%) and the adjusted breast cancer-related costs per person (€).
The Pearson correlation is also moderately positive and significant for lung cancer (r≈0.54, with its p-value≈0.005), prostate cancer (r≈0.47, with its p-value≈0.02) and breast cancer (r≈0.41, with its p-value≈0.04).
Assessing value in healthcare in cancer (VHC)
We will now combine the previous indicators in order to produce the VHC efficiency measures – that are reported in Table 1.
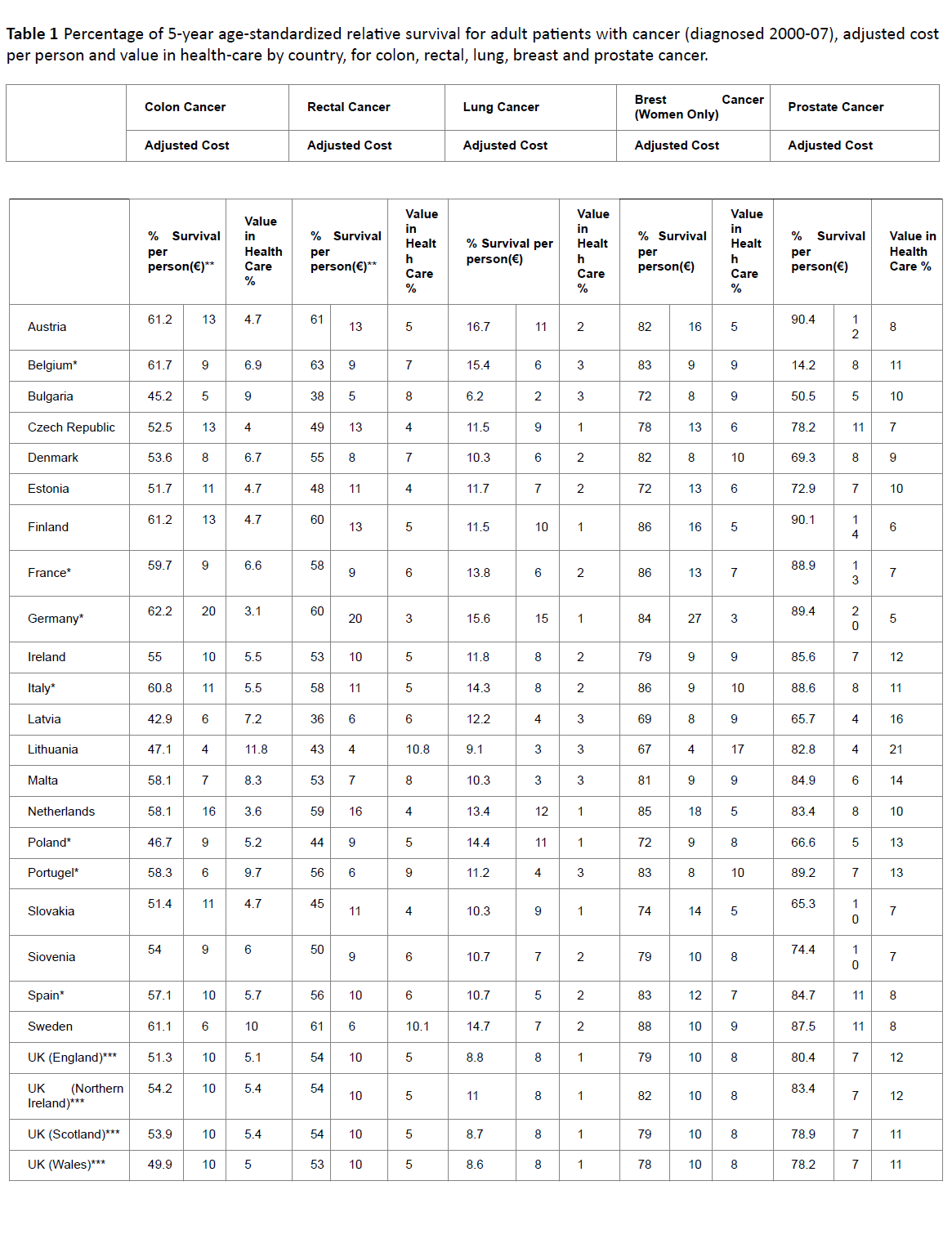
The initial columns of Table 1 compare the VHC for colon cancer. Lithuania, Sweden, Portugal, Malta and Bulgaria are the countries with a VHC above 8. France, Belgium, Slovenia, Denmark and Latvia have a VHC between 6 and 8. In the next group (lower than 6, but at least 4) are Spain, Italy, Austria, Czech Republic, Slovakia, Poland, Estonia, Finland, UK and Ireland. Germany and Netherlands present the lowest VHC.
The case of rectal cancer is similar and the comparison of countries’ rankings doesn’t differ very much, in spite of a slightly overall higher VHC in colon cancer (averages 6.3) versus rectal cancer (averages 6.0).
The VHC for lung cancer is very low in Poland, Czech Republic and Slovakia. The British islands are among the countries with a VHC under 1.5, as it happens in Germany, Netherlands and Finland. In the other Nordic countries, VHC stands between 1.5 and 2.5, in the same group as France and Austria (Central Europe) and Italy, Spain and Slovenia (Southern Europe). Portugal and Belgium are closer to 3 in their VHC and Malta has one of the highest values.
There are few regional standards in prostate cancer. Central Europe has good (Belgium and Netherlands), intermediate (Austria) and lesser results (Germany and France). In Southern Europe, Portugal and Italy have good VHC and Malta has the highest score, but Spain and Slovenia are below in the list. Northern Europe doesn’t achieve the 10-13 VHC group, and Finland is among the lowest ratios.
Finally, in breast cancer, VHC is higher in countries from different regions: Lithuania, Portugal and Denmark. Sweden (Northern), Latvia and Bulgaria (Eastern), Ireland (British islands), Italy and Malta (Southern) and Belgium (Central) have values between 8 and 10. The VHC of Spain, France, UK, Czech Republic, Poland and Slovenia varies between 6 and 8. With a few exceptions, Central Europe countries tend to have lower results in this indicator – this is an interesting matter of debate, due to clear differences in the wealth of these countries. The following section discusses these findings and implications in more detail.
Discussion
The concept of Value in Healthcare (VHC) should play a central role in the evaluation of the health-care systems. Some of the richest countries in Europe tend to achieve the best survival results in cancer. This isn’t a surprising conclusion, as it meets the idea that “successful health care system needs mainly financial investment”, [15] and this consistent investment is only possible in strong economies; but it’s questionable if this achievement results of efficient and effective health-care systems, or of overfunding. Inefficient systems can happen as result of many factors; inefficient human resource distribution may be an important one [12].
In order to propose an insightful and proper way to read VHC results, we will use some examples. In lung cancer survival, Germany ranks second, next only to Austria. But if we observe the following country on the list (Belgium), the survival rate is just 0.2 p.p. lower, achieved at a 9€ per person inferior cost. Germany’s VHC is 1€ per p.p., versus Belgium’s 2.6€ per p.p. This means that any extra euro per person with cancer-related costs represents a bonus of just 1 p.p. in lung cancer survival for Germans, while the same amount for person in Belgium would result in extra 2.6 p.p. of patients surviving the disease.
Likewise, Portugal is a poorer economy than its only land neighbor, Spain. Nevertheless, if we look, per example, to colon cancer, Portugal has better survival rate (58.3% versus 57.1%) at lower adjusted costs per person (6€ versus 10€). It is easy to realize Portuguese health-care system is working more efficiently and effectively than the Spanish one in colon cancer. But if the comparison was with the other main economy of southern Europe (Italy), what could we conclude? Italian survival is larger (60,8%), and its costs higher (11). Could we define Italian system, concerning colon cancer, better than Portuguese, based on survival? According to VHC analysis it is not more efficient – each Euro per Portuguese related to colon cancer cost represents 9.7% survival in the disease, against 5.5% in Italy. In fact, looking at overall results, Portugal is showing a great capability to manage its health resources in order to obtain the best results possible, considering lower investment power if compared to Spain or Italy.
By keeping our focus at an efficiency and efectiveness point of view, we can’t overlook the fact that, no matter which cancer we search, Germany has always the worst VHC. Also, there’s Lithuania’s tendency to top the VHC scores – usually by a large margin. Should one immediately conclude that Lithuania is on top of Europe’s cancer health-care system? Possibly no, illustrating why there should be a diversified “toolkit” for performing a multidimensional analysis on an healthcare system – of which VHC should be one instrument, due to its immediate relationship towards efficiency and effectiveness and the rich discussion on value-adding outcomes it involves. After all, in cancer, the ultimate goal is to assure long term survival for the patients, and with the best quality of life possible. So, we can’t just look at the VHC and evaluate the cancer health-care system of each country based on its results for the indicator. Lithuania tops the list for this indicator in all studied diseases except for lung cancer, but not as a consequence of good health-care, since their survival rates are under the average. Globally, Eastern Europe countries are part of a group whose VHC derives more from lesser spending in health than good allocation of resources. On the other hand, countries like Germany, Finland and Netherlands have negative results that we shouldn’t read as a sign that its cancer care system is an economic failure. We propose these numbers to be read as, e.g.: in Germany cancer health-care is less efficient than Belgium’s, despite its better survival numbers, because at the same level of adjusted costs per person, ceteris paribus, Belgium would achieve better results in lung cancer survival.
As a suggestion, this indicator should preferably be used as a comparative tool between countries with similar key variables: wealth or others. Comparing VHC between Germany and, for instance, the Baltic countries would be very delusive, and it couldn’t constitute an evidence of success by the healthcare system of the highest VHC country.
In Europe we can find different health care systems, and countries are organized in different ways in order to fight cancer. To what extent this differences can explained the results above? This is a very good question for future investigation.
Conclusion
This study focused on the efficiency and effectiveness – involving analyzing outcomes and costs – of European health care systems in their struggle against cancer. In particular, we proposed a measure called VHC which departs from the concept of value in healthcare as proposed by Porter, [12] and that this paper discussed and tested giving evidence of its potential and shortcomings.
We went further than exploring the relationship between costs and effects on cancer survival. We concluded the studied variables were correlated. Thus, their ratio (VHC) is an interesting indicator of the marginal impact an extra given amount invested in cancer has on the survival rate, as well as for ranking countries according to efficiency and effectiveness.
In a brief summary, from the empirical analysis, we can conclude that some countries, like Belgium and Portugal, tend to present a positive relation between costs and survival; others, as Lithuania, Latvia or Bulgaria also frequently present good ratios, but at the expense of very low spending and having under-average outcomes; and some, as Germany, Finland and Netherlands achieve acceptable survival rates in an inefficient way. As a result, we propose that this indicator to be used in the context of grained analysis, across countries of “similar” GDP per capita – or economic/political zones such as, the European Union or the USA.
On the whole, the VHC is a relevant instrument of analysis because it addresses to a major challenge in today’s provision of healthcare – the search for efficiency and effectiveness.
9500
References
- World Health Organization (2014) The 10 leading causes of death by income group (2011), Fact Sheet No. 310.
- Ades F, Senterre C, de Azambuja E, Sullivan R, Popescu R, et al. (2013) Discrepancies in cancer incidence and mortality and its relationship to health expenditure in the 27 European Union member states. Ann Oncol 24: 2897-2902.
- International Agency for Research on Cancer. (2014) Globocan 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012.
- https://ec.europa.eu/health/major_chronic_diseases/diseases/cancer/index_en.htm
- https://ec.europa.eu/health/major_chronic_diseases/diseases/cancer/index_en.htm#fragment1
- McGlynn E, Shekelle P, Chan S,Goldman DP, Romley JA,et al. (2008) Identifying, Categorizing, and Evaluating Health Care Efficiency Measures. Final Report (prepared by the Southern California Evidence-based Practice Center—RAND Corporation, under Contract No. 282-00-0005-21). AHRQ Publication No. 08-0030. Rockville, MD: AHRQ. 15: 5–6.
- Madore O. The Health Care System in Canada: Effectiveness and Efficiency. Librarv of Parliament, Research Division. Ottawa: Minister of Supply and Services.1994
- Luengo-Fernandez R, Leal J, Gray A, Sullivan R (2013) Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol 14: 1165-1174.
- De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, et al. (2014) Cancer survival in Europe 1999-2007 by country and age: results of EUROCARE--5-a population-based study. Lancet Oncol 15: 23-34.
- Ades F, Senterre C, de Azambuja E, Sullivan R, Popescu R, et al. (2013) Discrepancies in cancer incidence and mortality and its relationship to health expenditure in the 27 European Union member states. Ann Oncol 24: 2897-2902.
- Porter ME (2010) What is value in health care? N Engl J Med 363: 2477-2481.
- Björnberg A (2013) Euro Health Consumer Index Report 2013. Health Consumer Powerhouse 42: 16–17
- Gonçalves F (2011) A cross cou ntry explanation of performance of heath care systems: The consumer point of view using the Euro Health Consumer Index. Economic Modelling 28:196–200.