Vuignier, Sandra M.D.1 * , Tokairin, Kikutaro M.D.1, Aoyama, Takeshi M.D.1, Kobayashi, Hiroyuki M.D.1, Terasaka, Shunsuke M.D.1, Hida, Kazutoshi M.D.1, Houkin, Kiyohiro M.D.1
1Department of Neurosurgery, Hokkaido University Hospital, Japan.
*Corresponding Author:
Vuignier, Sandra M.D
Department of Neurosurgery, Hokkaido University Hospital, Japan.
E-mail: sandravuignier@gmail.com
Keywords
bone metastasis, extraneural metastasis, glioblastoma multifore, paraparesis, PET study.
Introduction
Gliomastoma multiforme, a high malignant tumor originating from astrocytes, accounts for one fifth of all brain tumors. The prognosis is poor with an average survival time of approximately 1 year [2, 3].
GBM is a tumor with a strong tendancy for local invasion, with a high rate of local relapse after surgical excision and leptomeningeal seeding. However, dissemination outside the central nervous system (CNS) is quite unusual, with a reported incidence of barely 2% and an occurrence late in the course of the disease, after a median of 2 years [9]. The literature showed that the most frequent site of the primary tumour was supratentorial and metastasis disstribution was in lungs, pleura, lymph nodes, bones and liver [10]. Smith et al. [18] reported a 0.44% incidence of extracranial metastases from GBMs among the 8000 primary brain tumors included in their study, and Pasquier, et al. [14], found 72 cases of this kind after reviewing the world literature dated through 1977. Here we descrived a very rare case of a 70 years old man with a metastasis from a cerebral GBM to the vertebral bodies of the thoraci levels.
Case report
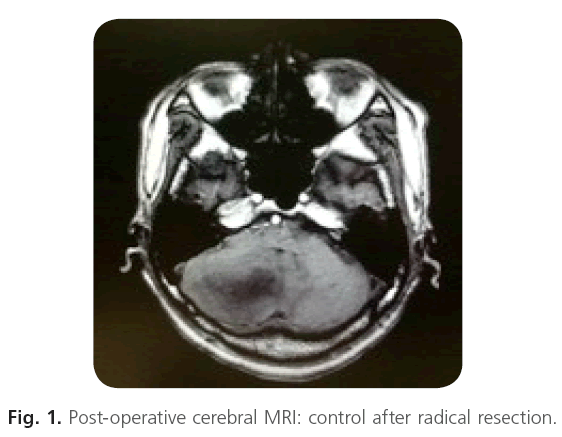
We report a case of a 70-year-old man with antecedents of tuberous sclerosis, hepatite C and craniotomy for removal of a right cerebellar tumor. The brain surgery was performed in another hospital and the pathology was a glioblastoma multiforme. The lesion was fully resected macroscopically (Figure 1).
Figure 1: Post-operative cerebral MRI: control after radical resection.
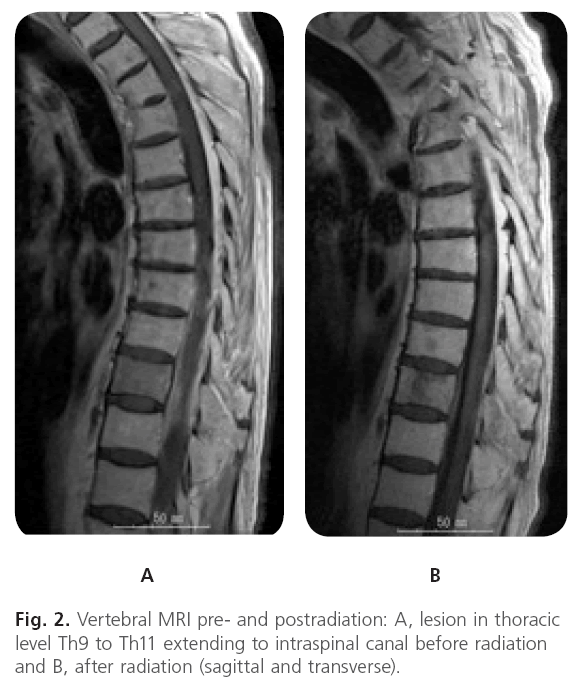
After the surgery the patient was treated with temodozamide (TMZ) and radiotherapy by local irradiation of 60 Grays (Gy) in 30 fractions. He then received TMZ once a week as an out-patient. 6 months after the surgery he presented lumbago. From next day he showed weakness of bilateral lower extremities, therefore, he admitted our referred hospital again. However he bacame paraplegic within a day. A MRI on admission showed a diffuse lesion at the thoracic levels from Th9 to Th11 and compression of the spinal cord (Figure 2A). Because of the compression of the spinal cord, the clinical findings and the age of the patient we administrated in emergency a local radiation of 25 Gy in 5 fractions. A post-radiation vertebral MRI demonstrated a decreased in size of the lesion (Figure 2B).
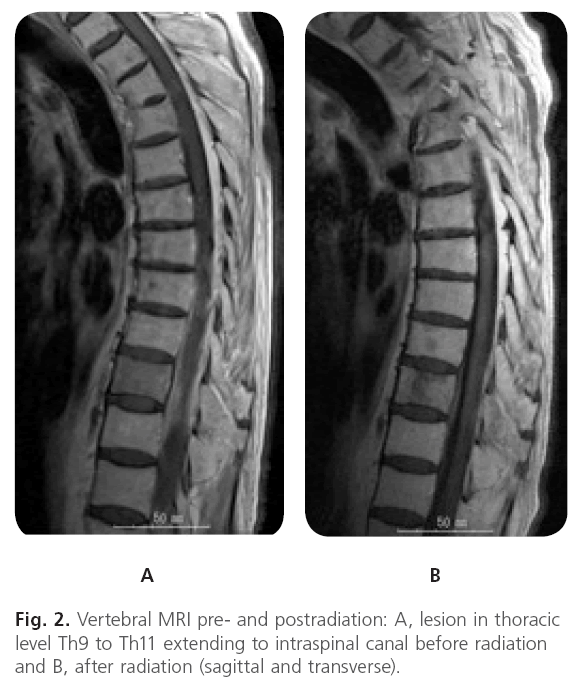
Figure 2: Vertebral MRI pre- and postradiation: A, lesion in thoracic level Th9 to Th11 extending to intraspinal canal before radiation and B, after radiation (sagittal and transverse).
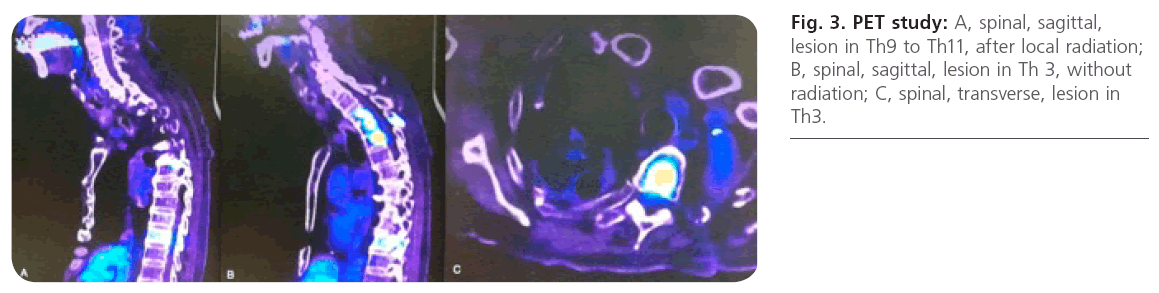
We completed the oncologic bilan with a PET study. The PET study show a reduction of signal in Th9 to Th11 but also revealed a new lesion in the thoracic level extending from Th2 to 4 (Figure 3).
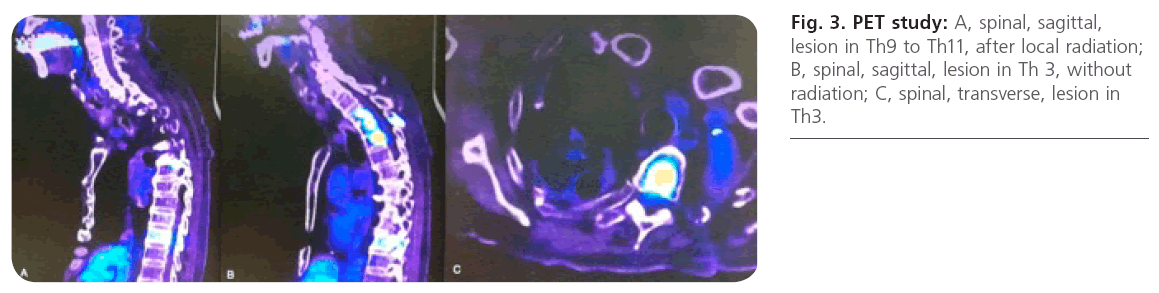
Figure 3: PET study: A, spinal, sagittal, lesion in Th9 to Th11, after local radiation; B, spinal, sagittal, lesion in Th 3, without radiation; C, spinal, transverse, lesion in Th3.
A biopsy was performed at this new level. The pathology came back to be a GBM with the same small cells and characteristics of the GBM previously in the brain. The patient was then treated by ACNU-based chemotherapy for recurrent glioma in the TMZ era.
Discussion
Malignant gliomas account for approximately 60% of all primary brain tumors in adults. Development of systemic metastasis from primary intracranial gliomas is rare, but the observed frequency of extracranial metastasis has recently been increasing; on the other hand, this increased incidence has been accompanied by longer patient survival times because of advances in the treatment of gliomas [1]. Glioblastomas can metastase to the pleura and/or lung in 60%, to the lymph nodes in 51%, to the bones in 31% and to the liver in 22% [14]. Extraneural metastasis are rare with an incidence less than 2 % [1]. Concerning bone metastasis, Pasquier et al. [14], reported that the vertebral spine (73%) was the most frequent site of involvement, followed by the ribs in 23%, the sternum in 18%, the skull in 14% and the acetabulum in 9% [14]. Bone lesions may be radiographically osteolytic, osteoblastic or mixted [4, 7, 8, 12, 15].
Although bone metastasis from GBM are very rare they have been already reported in the litterature. It is worth pointing out the aspects in which our case differs from previously reported cases. The site, vertebral spine, of the bone metastasis in our patient was similar to those of all the previously reported cases. However, our patient was relatively old, and the extraneural metastasis occurred relatively ealier in the evolution of the disease (after 6 months). The average patient age associated with GBM related metastasis has been demonstrated to be around 35.8 years [14, 20], which is very different from the age of our patient who is nearly the double. Moreover, it has been showed that extraneural metastasis from brain tumors occur late in the course of the disease, after a median of 2 years, which was not either the case in our patient [9] that was diagnosed as having a metastasis only after half a year.
Most cases have of metastasis have been showed to come from the supratentorial part of the brain [10]. Our patient have a metastasis that comes from the infratentorial part of the brain, the cerebellum. We search in the literature for metaststasis of cerellar GBM and found only one case, published before, by Fabi et al. [6]. The clinic is also rare. A review of the world’s literature performed by Chesnut et al. [4] for reported cases of histologically proven metastasis of glial tumors to the vertebrae documented in 28 cases [4, 5, 8, 11, 15, 16, 17, 18, 19, 21]. Over half of these cases have been asymptomatic (60.7%), 11 (39%) have been complaining of pain in the region of the axial skeleton involved by the tumor and only 3 (0.3%) have been presenting with accompanying neurological deficit [19]. Another rare fact is that there is no recurrence of the tumor in the brain although there are metastasis discovered in more than one level in the verebral bone. It is very rare to have distant metastasis without cerebral tumor relapse, only one case as been published before, by Fabi et al. [6].
The study by PET is also very interesting. To our knowledge this is the first case reported of extraneural bone metastasis from a cerebral GBM demonstrated on a whole body PET study (Figure 3). On the different pictures we can see that there is no recurrence in the brain and no new tumor or metastasis in the brain. The thoraic levels Th9 to Th11 that have been radiated locally before show no intense signal in the contrary to the levels Th2 to Th 4 that highlight an intense signal. Extraneural metastasis tend to metastase to multiples body regions as soon solitary metastasis have been reported. It is important to follow-up surviving glioma patients in order to treat them in time.
Conclusion
We reported a very rare case of a metastasis to the thoracic levels from a cerebellar GBM in an old patient. Radical excision, radiation therapy and chemotherapy should be applied as soon as possible in primary glial tumors. With respect to occult or remote metastasis, patients should be scanned particulary using contrast – enhanced MRI with Gd. PET Study is useful to detect other metatasis. Importantly we need to keep following this patient. A longer follow-up of the surviving glioma patients is mandatory to disclose and understand the changes which include extraneural metastasis.
1952
References
- Beauchesne, P., Soler, C., Mosnier, JF. Diffuse vertebral body metastasis from a glioblastoma multiforme: A technetium-99m Sestamibi single-photon emission computerized tomography study. J Neurosurg. 2000 ; 93: 887-890.
- Chesnut, RM., Abitbol, JJ., Chamberlain, M., Marsall, LF. Vertebral collapse with quadraparesis due to metastatic glioblastoma multiforme: A case report and review of the literature. J Neuro- Onco. 1993; 16: 135-140.
- Dietz, R., Burger, L., Merkel, K., Schimrigk, K. Malignant glioblastomas-glioblastom multiforme and astrocytoma IIIIV with extracranial metastases. Report of two cases. Acta Neurochir. 1981; 57: 99-105.
- Fabi, A., Vidiri, A., Carapella, C., Pace, A., Occhipinti, E., Caroli, F., Mirri, A. et al. Bone Metastasis from Glioblastoma Multiforme Without Central Nervous System Relapse: A Case Report. Anticancer Research 2004; 24: 2563-2566.
- Gamis, AS., Egelhoff, J., Roloson, G., Young, J., Woods, GM., Newman, R., Freeman, AI. Diffuse bony metastases at presentation in a child with glioblastoma multiforme. A Case Report. Cancer 1990; 66: 180-184.
- Haddon, M., Slavin, JD., Spencer, RP. Multiple bone metastases in a patient with glioblastoma multiforme. Clin Nucl Med. 1989; 14: 13-14.
- Hoffman, HJ., Duffner, PK. Extraneural metastases of central nervous system tumors. Cancer 1985; 56 (Suppl.): 1178-1182.
- Kumar, R., Jain, R., Tandon, V. Thalamic glioblastoma with cerebrospinal fluid dissemination in the peritoneal cavity. Pediatr Neurosurg 1999; 31: 242-245.
- Lampl, Y., Eshel, Y., Gilad, R., Sarova, PI. Glioblastoma multiforme with bone metastases and cauda equina syndrome. J Neurooncol 1990; 8: 167-172.
- Myers, T., Egelhoff, J., Myers, M. Glioblastoma multiforme presenting as osteoblastic metastasic disease: Case report and review of the literature. Am J Neuroradiol. 1990; 11: 802-803.
- Pang, D., Ashmead, JW. Extraneural metastasis of cerebellar glioblastoma multiforme. Neurosurgery 1982; 10: 252-257.
- Pasquier, B., Pasquier, D., N’Golet, A. Extraneural metases of astrocytomas and glioblastomas. Clincopathological study of two cases and review of the literature. Cancer 1980; 45: 112- 125.
- Sadik, AR., Port, R., Garfinkel, B., Bravo, J. Extracranial metastasis of cerebral glioblastoma multiforme: Case report. Neurosurgery 1984; 15: 549-551.
- Shuster, H., Jellinger, K., Grund, A., Regele, H. Extracranial metastases of anaplastic cerebral glioma. Acta Neurocir. 1976; 35: 247-259.
- Shinumra, F., Chen, M., Itoh, T., Ariwa, R. An autopsy case of extraneural metastases of giant cell glioblastoma with intracerebral hemorrhage. No Shinkei Geka 1985; 13: 1245- 1250.
- Slowik, F., Balogh, I. Extracranial spreading of glioblastoma multiforme. Zentralbl Neurochir 1980; 41: 57-68.
- Vural, G., Hagmar, B., Walaas, L. Extracranial metastasis of glioblastoma multiforme diagnosed by fine needle aspiration: A report of two cases and review of the literature. Diagn Cytopathol. 1996; 15: 60-65.
- Wisiol, ES., Handler, S., French, LA. Extracranial metastases of a glioblastoma multiforme. J Neurosurg. 1962; 19: 186-194.