Review Article - (2022) Volume 16, Issue 3
Vitamin D Deficiency As A Risk Factor For Mortality In Critically Ill Patients.
Bryan Fernando Salazar Ibarra,
Jennifer Cristina Carvajal Ojeda,
Carmen Chamorro Acevedo,
Marco Antonio Ditta Cassiani and
Esteban Gomez Rios
General Physician, Universidad Cooperativa de Colombia, Colombia
Universidad de las Americas, Ecuador
General Physician, Universidad Nacional de Loja, Ecuador
General Physician, Universidad Nacional de Loja, Ecuador
1General Physician, Universidad Cooperativa de Colombia, Colombia
General Physician, Universidad Libre, Colombia
2General Physician, Universidad Metropolitana, Colombia
General Physician, Universidad Cooperativa de Colombia, Colombia
*Correspondence:
Cristian Camilo Burbano Insuasty, General Physician, Universidad Cooperativa de Colombia,
Colombia,
Email:
Received: 30-Mar-2022, Manuscript No. iphsj-22-12581;
Editor assigned: 01-Apr-2022, Pre QC No. Preqc No: iphsj-22-12581;
Reviewed: 17-Apr-2022, QC No. QC No. iphsj-22-12581;
, Manuscript No. iphsj-22-12581(R);
Published:
25-Apr-2022, DOI: 10.36648/1791-809X.16.4.932
Abstract
Background: Vitamin D is produced in the skin upon sun exposure. Vitamin D is necessary to maintain serum calcium concentration within the normal physiologic range for musculoskeletal health. Currently one in five Americans dies in the ICU, and virtually every generation today will have an ICU encounter in their lifetime. Survivors of critical illness are at risk for subsequent hospitalization, outpatient evaluation and related health care costs.
Methodology: A systematic review was carried out through various databases from January 2010 to February 2022; the search and selection of articles was carried out in indexed journals in English. Key words used were: Vitamin D, Mortality, ICU, Critical patient.
Results: Vitamin D3 is produced in the skin from 7-dehydrocholesterol in a two-step process in which the B-ring is broken down under ultraviolet rays (e.g., sunlight) and the pre-D3 formed in this process is isomerized to D3 in a sensitive but non-catalytic thermo- process. Vitamin D deficiency could lead to major health impacts, including higher severity of illness scores and risk of death, longer ICU stay, longer duration of mechanical ventilation, higher rates of ventilator-associated pneumonia and positive blood cultures, and a higher incidence of organ dysfunction, particularly acute kidney injury.
Conclusions: The present review provides current and accurate information on the functions of vitamin D, what its deficiency entails and its impact on health and its role as a risk factor for mortality in critically ill patients.
Keywords
Vitamin D; Mortality; ICU; Critical patient; ICU; mortality
Introduction
Vitamin D is labeled as the "sunshine vitamin" because it is
produced in the skin upon exposure to the sun. Vitamin D is
necessary to maintain serum calcium concentration within the
normal physiologic range for musculoskeletal health [1].
The Endocrine Society, the National and International
Osteoporosis Foundation and the American Geriatric Society
define vitamin D deficiency as a 25-hydroxyvitamin (25 OH D)
level below 30 ng/mL. The Endocrine Society recommends a
preferred range of 40 to 60 ng/mL [2].
Vitamin D deficiency in children causes rickets and prevents
children from reaching their maximum bone mass and genetically
determined height. In adults, vitamin D deficiency causes
abnormal mineralization of the collagen matrix in bone, known
as osteomalacia. This collagen matrix is weak, does not provide adequate structural support, and increases the risk of fracture
[3].
Vitamin D is a hormone obtained through dietary intake and skin production. Ultraviolet B (UVB) radiation, wavelength (290 to
315 nm) converts 7- dehydrocholesterol in the skin to provitamin
D. [4, 5] This provitamin D undergoes isomerization by heat
and is converted to vitamin D. Vitamin D from skin and diet is
metabolized in the liver to 25-hydroxyvitamin D (25 OH D), and
25-hydroxyvitamin D is useful for assessing vitamin D status. [5].
In the 1950s and 1960s, when the field of critical care developed,
the primary focus was on survival: taking a patient who was dying
imminently, providing vital organ support with infusions and
pharmaceutical machines, and saving the patient from the agony
of death [5, 6].
Currently one in five Americans dies in the ICU, and virtually all
of today's generation will have an ICU encounter during their
lifetime. Survivors of critical illness are at risk for subsequent
hospitalization, outpatient evaluation, and related health care
costs [6, 7] It is therefore appropriate to undertake this work
in order to provide current and accurate information on the
functions of vitamin D, what its deficiency entails and its impact
on health and its role as a risk factor for mortality in critically ill
patients.
Materials and Methods
A systematic review was carried out, searching PubMed, Scielo
and Science Direct databases, among others. The collection
and selection of articles was carried out in English-language
indexed journals from 2010 to 2022. As keywords, the following
terms were used in the databases according to DeCS and MeSH
methodology: Vitamin D, Mortality, ICU, Critical patient. In this
review, 80original and review publications related to the topic
studied were identified, of which, articles28 met the specified
inclusion requirements, such as, articles that were in a range not
less than 2010, that were full text articles and that reported on
vitamin D as a factor in the mortality of critical patients. Mortality
risk in critically ill patients. Exclusion criteria took into account
that the articles did not have sufficient information and that they
did not present the complete text at the time of review.
Results
Results Vitamin D
Vitamin D3 is produced in the skin from 7-dehydrocholesterol in
a two-step process.
Stages in which the B-ring is cleaved under ultraviolet rays (e.g.,
sunlight) and the pre-D3 formed in this process is isomerized to
D3 in a sensitive but non-catalytic thermo-process [8].
The three main steps in vitamin D metabolism, 25-hydroxylation,
1a-hydroxylation and 24- hydroxylation are carried out by
cytochrome P450 mixed function (CYP) oxidases. The first step
toward activation is the conversion of vitamin D to 25-hydroxy-D.
[9] In addition to UV activation, small amounts of vitamin D,
either as D2 or D3, can enter the body from intestinal absorption
from dietary intake and progress to activation by hydroxylation
[10].
The next step towards full activation is dihydroxy-vitamin1, 25 D
(1, 25 (OH) 2 D) Through CYP27B1 (also known as 1-alpha hydroxylase), a
mitochondrial P450 enzyme in the proximal renal tubule of the
kidney. 25-hydroxyvitamin D 24 hydroxylase, also known as
CYP24, can hydroxylase both 25-hydroxy-D and 1, 25(OH) 2 D.
In addition to 1, 25(OH) 2 D, the kidney also produces 24, 25
dihydroxyvitamin D, a relatively inactive metabolite [11].
Functions of Vitamin D
(OH) D. The regulation of this conversión at the tissue level differs
from the conventional activation occurring in the kidney in that
it is more substrate dependen and, therefore, more susceptible
to vitamin D deficiency. [12, 13], The non-skeletal actions of
vitamin D are mediated by the control of gene expression in a
number of organs such as brain, prostate, colon and immune
cells, which may be of particular relevance in critical illness
[14]. These non-skeletal actions result in the regulation of cell
proliferation, differentiation, apoptosis and angiogénesis. In
fact, the mechanism of action of vitamin D in these contexts is
analogous to the way steroid hormones act. As a result of this
contemporary knowledge, vitamin D is considered more of a
hormone than a vitamin. In we can see other functions of vitamin
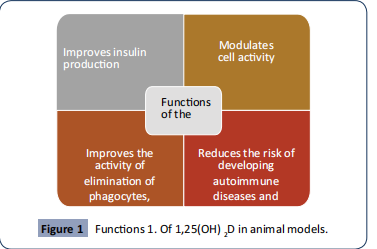
D found in animal models. [14-18] (Figure 1)
Figure 1 Functions 1. Of 1,25(OH) 2D in animal models.
Vitamin D Deficiency And Its Impact On Health
Several population studies have shown that low vitamin D
levels are associated with poor outcomes. However, causality is
more difficult to establish given that a low vitamin D level itself
could be a marker of poor general health and deficiency is seen
in people with limited physical activity and little exposure to
sunlight, advanced age, obesity, poor diet, and other comorbid
diseases [19].
In the general population, mortality risk appears to decrease
with increasing 25 hydroxy-D levels, with optimal levels of 75 to
87.5 nmol/l. A large meta-analysis of community dwelling adults
showed that the lowest observed 25-hydroxy-D quintile was
associated with increased mortality [19].
Conditions that have been associated with vitamin D deficiency
include certain malignancies such as colon, breast, ovarian,
prostate, and lymphoma. Some studies also report an increased
risk of mortality with these cancers in people with vitamin D
deficiency [20].
Similarly, low vitamin D levels have been associated with
cardiovascular conditions, such as poor control of hypertension
and congestive heart failure [21].
Subjects with vitamin D deficiency who have multiple sclerosis,
diabetes, depression, and certain infections such as influenza,
tuberculosis, and other conditions have shown a similar
association with adverse outcomes. [21]. Several observational
studies in critically ill patients have shown an association between
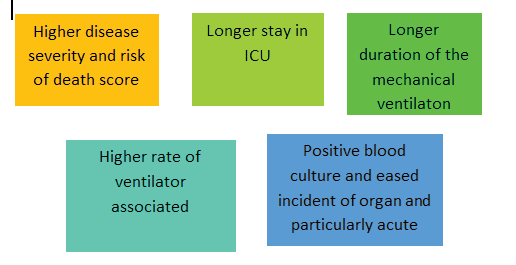
vitamin D deficiency and adverse outcomes, in Figure 2 we can
identify the main conditions [19-23] (Figure 2).
Figure 2 Main conditions of vitamin D deficiency in critically
ill patients.
Associated ICU and hospital costs are also higher in patients with
vitamin D deficiency [20].
Vitamin D supplement Hnigtahteior nraitseos no of the thera
npdeuatnicinsctraetaesgeides implemented in this type of
patients, among thpenemumosotnfiraequently report eddy
safudnvectrisoene, effects is mild hyperkalaemia [23, 24].
Vitamin D deficiency in critical illness has been associated with
poor outcomes and increased mortality. Although there are
biologically plausible mechanisms by which vitamin D deficiency
in critical.
Which deficiency could contribute to these outcomes, such as
immune dysfunction, cardiovascular disease, dysglycemia, and
endothelial and mucosal barrier disruption [25]
It is possible, therefore, that the low levels observed are simply
a marker of poor overall health resulting in limited sunlight
exposure, chronic disease, and poor diet and, therefore, are
associated with adverse outcomes with vitamin D deficiency being the innocent by stander of this inevitable trajectory [15].
Therefore, vitamin D deficiency could not be considered as
the cause of the clinical picture of the patient, but rather the
detection of this vitamin could contribute to determine the
patient's prognosis. In Table 1 we can identify other functions
of vitamin D in different organs [12, 27, 22, 23,25, 26]. (Table 1).
| Organ |
Function |
| Immune system |
Vitamin D metabolites act as modulators of innate and adaptive system cells. |
| Cardiac function |
Vitamin D may play a role in the prevention of atrial fibrillation by negatively regulating the renin-angiotensin- aldosterona system (RAAS), mediating calcium homeostasis, binding to vitamin D receptors (VDRs) on cardiac myocytes and, in addition, having antioxidant properties that may reduce levels of reactive oxygen species (ROS) in the atria, which contribute to inflammation and the formation of proarrhythmic substrates. |
| Pulmonary function |
Lack of vitamin D receptors in the barrier. Epithelial lung tissue appeared to compromise its defense, which Caused more severe lipopolysaccharide (LPS)-induced lung injury. Thus, vitamin D could be a therapeutic approach in different types of lung conditions. |
|
| Function muscular metabolic |
Some animal models have confirmad that the Vitamin D deficiency and congenital abnormalities in the vitamin D endocrine system can cause muscle weakness. |
| Bone |
Limited available data in ICU survivors suggest impaired bone health and a high risk of fracture in patients with vitamin D deficiency. |
Table 1. Vitamin D identify other functions of vitamin D in different organs.
Discussion
The retrospective study of a medical intensive care unit in a
community hospital by Sindhaghatta et al report on a large
cohort of patients with 25(OH) D deficiencies and insufficiency
in an ICU setting. This study shows a clear association between
25(OH)D levels and hospital mortality in critically ill patients.
25(OH) D levels of 10 ng/dL predicted hospital mortality in 83.6%
of this cohort. The hospital mortality observed for patients with
25(OH)D deficiency was higher than the mortality predicted by
the APAC HE IV score on admission [27]
Another study by Rafael et al, in which they prospectively
measured vitamin D on admission of 125 intensive care unit
patients, and weekly until discharge from the ICU, analysing the
parameters of 28-day mortality, mechanical ventilation, length
of stay, infection rate and culture positivity. They concluded That
low vitamin D levels on ICU admission are an independent risk
factor for mortality in critically ill patients and that low vitamin
D levels on ICU admission may have a causal relationship with
mortality and may serve as a marker for vitamin D replacement
among critically ill patients [28].
Strength of the current study is the methodology implemented,
with respect to the literature search, and steps in the selection
of relevant articles, quality assessment and data extraction.
However, this study has several limitations, which should be
taken into account before reaching a conclusion, among these
are the little evidence of clinical trial analysis to determine the
relationship between deficiency and the percentage of mortality
in patients hospitalized in an intensive care unit, hospitalized in
general ward or critical patients, so more studies are needed to
answer these questions.
Conclusion
Vitamin D3 is produced in the skin from 7-dehydrocholesterol in a
two-step process in which the B-ring is cleaved under ultraviolet rays (e.g., sunlight) and the pre-D3 formed in this process is
isomerized to D3 in a thermo-sensitive but non-catalytic process.
There is a growing appreciation of the many functions of
vitamin D beyond its classic actions on calcium metabolism and
musculoskeletal health.
The non-skeletal actions of vitamin D are mediated by the control
of gene expression in a number of organs such as brain, prostate,
colon and immune cells, which may be of particular relevance in
critical diseases. There are other functions of Vitamin D described
in animal models, such as Enhances insulin production, Modulates
T and B cell activity, Enhances the activity of elimination of
phagocytes, improves vascular smooth muscle resistance and
reduces the risk of developing autoimmune diseases and inhibits
the growth of cancer cells.
Vitamin D deficiency could have a major impact on health,
including higher severity of illness scores and risk of death, longer
ICU stay, longer duration of mechanical ventilation, higher rates
of ventilator-associated pneumonia and positive blood cultures,
and a higher incidence of organ dysfunction, particularly acute
kidney injury.
REFERENCES
- Stamm E, Acchini A, Da Costa A, Besse S, Christou F (2019) Year in review: geriatrics. Rev Med Suisse 09:50-52.
Indexed at, Google Scholar
- Hernigou P, Auregan JC, Dubory A (2019) Vitamin D: part II; cod liver oil, ultraviolet radiation, and eradication of rickets. Int Orthop 43:735-749.
Indexed at, Google Scholar, Crossref
- Tang H, Li D, Li Y, Zhang X, Song Y et al. (2018) Effects of Vitamin D Supplementation on Glucose and Insulin Homeostasis and Incident Diabetes among Nondiabetic Adults: A Meta-Analysis of Randomized Controlled Trials Int J Endocrinol 7908764.
Indexed at, Google Scholar, Crossref
- Fink C, Peters RL, Koplin JJ, Brown J, Allen KJ (2019) Factors Affecting Vitamin D Status in Infants. Children 6.
Indexed at, Google Scholar, Crossref
- Häusler D, Weber MS (2019) Vitamin D Supplementation in Central Nervous System. Demyelinating Disease-Enough Is Enough Int J Mol Sci 8:20.
Indexed at, Google Scholar, Crossref
- Awadh AA, Hilleman DE, Knezevich E, Malesker MA, Gallagher JC (2003) Vitamin D supplements: The pharmacists' perspective J Am Pharm Assoc 61:e191-e201.
Indexed at, Google Scholar, Crossref
- Teymoori-Rad M, Shokri F, Salimi V, Marashi SM (2019) The interplay between vitamin D and viral infections. Rev Med Virol 29:e2032.
Indexed at, Google Scholar, Crossref
- Halpern NA, Shepherds SM (2010) Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med 38:65-71.
Indexed at, Google Scholar, Crossref
- Ruhl AP, Huang M, Colantuoni E, Karmarkar T, Dinglas VD (2017) Healthcare utilization and costs in ARDS survivors: a 1-year longitudinal national US multicenter study. Intensive Care Med 43:980-991.
Indexed at, Google Scholar, Crossref
- Haas B, Wunsch H (2016) How does prior health status (age, comorbidities and frailty) determine critical illness and outcome? Curr Opin Crit Care 22:500-505.
Google Scholar, Crossref
- Wilson ME, Barwise A, Heise KJ (2018) Long-term return to functional baseline after mechanical ventilation in the ICU. Crit Care Med 46:562-569.
Indexed at, Google Scholar, Crossref
- Pandharipande PP, Girard TD, Jackson JC (2013) Long-term cognitive impairment after critical illness. N Engl J Med 369:1306-1316.
Google Scholar
- Ferrante LE, Murphy TE, Gahbauer EA (2018) Pre-ICU cognitive status, subsequent disability, and new nursing home admission among critically ill older adults. Ann Am Thorac So 15:622-629.
Indexed at, Google Scholar, Crossref
- Bikle DD (2014) Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol 21:319-329.
Indexed at, Google Scholar, Crossref
- Ray R, Banks M, Abuzahra H, Eddy VJ, Persons KS et al. (2012) Effect of dietary vitamin D and calcium on the growth of androgen-insensitive human prostate tumor in a murine model. Anti cánc Res 32:727-731.
Indexed at, Google Scholar
- Palacios C, Gonzalez L (2014) Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol 144:138-145.
Indexed at, Google Scholar, Crossref
- Shaman J, Jeon CY, Giovannucci E, Lipsitch M (2011) Short comings of vitamin D-based model simulations of seasonal influenza. PLoS One.6:e20743.
Google Scholar, Crossref
- Autier P, Boniol M, Pizot C, Mullie P (2014) Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol 2:76-89.
Indexed at, Google Scholar, Crossref
- Schottker B, Jorde R, Peasey A, Thorand B, Jansen EH et al. (2014) Vitamin D and mortality: meta-analysis of individual participant data from a large consortium of
Cohort studies from Europe and the United States. BMJ 348:g3656.
Google Scholar
- Anglin RE, Samaan Z, Walter SD, McDonald SD (2013) Vitamin D deficiency and depression. in adults: systematic review and meta-analysis. Br J Psychiatry 202:100-107.
Indexed at, Google Scholar, Crossref
- Huang SJ, Wang XH, Liu ZD, Cao WL, Han Y et al. (2017) Vitamin D deficiency and the risk of tuberculosis: a meta-analysis Drug Des Devel Ther 11:91-102.
Google Scholar, Crossref
- Nair P, Lee P, Reynolds C, Nguyen ND, Myburgh J et al. (2013) Significant perturbation of vitamin D-parathyroid-calcium axis and adverse clinical outcomes in critically ill patients. Intensive Care Med 39:267-274.
Indexed at, Google Scholar, Crossref
- Moromizato T, Litonjua AA, Braun AB, Gibbons FK, Giovannucci E et al. (2014) Association of low serum 25-hydroxyvitamin D levels and sepsis in the critically ill. Crit Care Med 42:97-107.
Indexed at, Google Scholar, Crossref
- Quraishi SA, Bittner EA, Blum L, McCarthy CM, Bhan I (2014) Jr Prospective study of vitamin D status at initiation of care in critically ill surgical patients and risk of 90-day mortality. Crit Care Med 42:1365-1371.
Indexed at, Google Scholar, Crossref
- de Haan K, Groeneveld AB, de Geus HR, Egal M, Struijs A (2014) Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: systematic review and meta-analysis. Crit Care 18:660.
Indexed at, Google Scholar, Crossref
- McNally JD, Nama N, O'Hearn K, Sampson M, Amrein K et al. (2017) Vitamin D deficiency in critically ill children: a systematic review and meta-analysis. Crit Care 21:287.
Google Scholar, Crossref
- V. Sindhaghatta, C. Sridhar, A. Muhammad (2011) Vitamin D deficiency is associated with mortality in the medical intensive care unit. Crit Care R292.
Indexed at, Google Scholar, Crossref
- B. Rafael, F. Gilberto, C. Iuri (2015) Vitamin D deficiency is independent associated with mortality among critically ill patients. Clinics 70: 326-332.
Google Scholar, Crossref
Citation: nsuasty CCB, Guzmán LFC, Ibarra BFS, Ordóñez RRC, Ojeda JCC, et al. (2022) EVitamin D Deficiency As A Risk Factor For Mortality In Critically Ill Patients. Health Sci J. Vol. 16 No. 3: 932.