Beatriz Losada Vila*, David Gutiérrez Abad, Maria Victoria de Torres Olombrada, Ignacio Juez Martel, Laura Rodriguez Lajusticia, Diego Malón Giménez, Maria del Carmen Pantin González and Juan Antonio Guerra Martínez
Hospital University of Fuenlabrada, Calle Camino del Molino, Fuenlabrada, Madrid, Spain
- *Corresponding Author:
- Beatriz Losada Vila
Hospital University of Fuenlabrada, Calle Camino del Molino
2, 28942 Fuenlabrada, Madrid, Spain
Tel: 65554555655
E-mail: beatriz.losada@salud.madrid.org
Received Date: 10 May 2017; Accepted Date: 31 May 2017; Published Date: 05 June 2017
Citation: Vila BL, Abad DG, Olombrada MVT, et al. When Constipation is not due to Opioids and the Management of Pain is not Proper: Implications in Cancer Treatment. Ann Clin Lab Res. 2017; 5:2. DOI: 10.21767/2386-5180.1000171
Keywords
Constipation; Cancer treatment
Introduction
Pain is a common symptom in oncological patients, with more than 70% of them not well controlled. It also decreases quality of life, so it is very important that Medical Oncologists know about pain etiology. Many factors can be worsening in pain control, since chemotherapy (neuropathic pain) to moving, eating. Therefore, management of opioids require a good knowledge about side effects with the aim of not to stop opioids when they appear.
In this case report we will review the management of different pain types and indications of titration or rotation opioids, taking into account elderly patient´s fragility and family education [1].
Case Report
A 73-year-old patient with a personal background of smoker 60 cigarettes a day. He went to the emergency room (January 2015) after presenting a weight loss of 7 kg in the last 6 months and cough without expectoration or hemoptysis. He also presents progressive coxalgia that limits moving from 3 weeks ago, so he started Targin 20 mg/10 mg (Oxycodone/ Naloxone) and deficiency anemia so he was on iron therapy.
In the physical examination, just two left inguinal adenopathies (1 cm). Impressions of dysesthesia at L1-L3 territory.
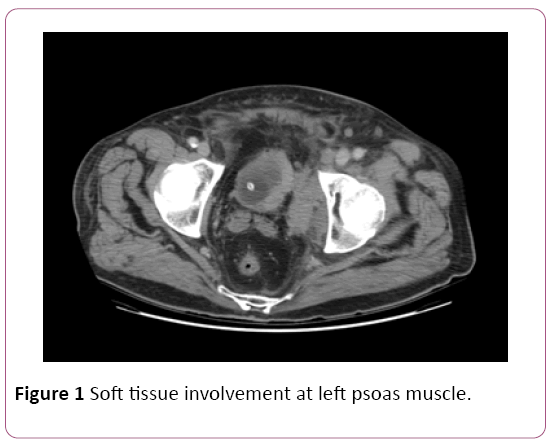
Additional tests showed the following results. Analysis only were relevant because of anemia: Hb 9.7 g/dl. CT thoracicabdominal- pelvis: mass of 5 × 4 cm in right lung, compatible with lung cancer. Abundant feces in a non-obstructive pattern. Soft tissue involvement at left psoas muscle (Figure 1).
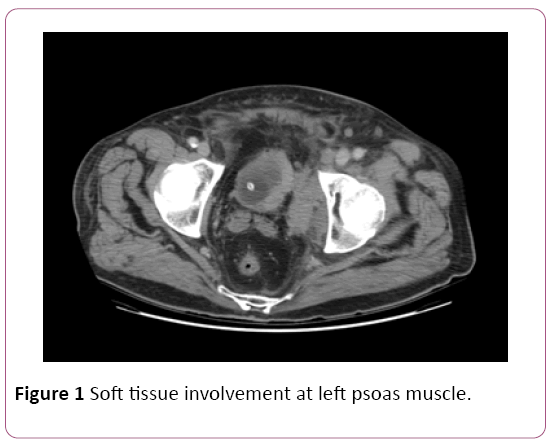
Figure 1: Soft tissue involvement at left psoas muscle.
He was admitted to further study. Abdominal pain was probably multifactorial: chronic constipation exacerbated by the use of opioids + iron and intestinal sub obstruction.
Somatic nociceptive pain referred to left hip was mostly common due to metastatic involvement. Lung and bone biopsies confirmed small cell lung cancer, so diagnosis was a small lung cancer stage IV, deciding palliative treatment.
At first days, abdominal pain improved after starting laxatives. However, hip pain made him difficult to move, so constipation got worse again and he started vomiting. Internal Medicine Doctor assumed constipation relation to opioids and rotated oxycodone/naloxone 20 mg/10 mg to a fentanyl patch of 12 mcg/72 hours (equivalent dose would be 17 mcg, however they decide a lower dose due to secondary effects) [1-3].
However, at next day, he again reported an episode of dizziness and 2 vomits, with instability in bed and poor control of pain since switch to fentanyl patch. Internal Medicine Doctor decided to titrate with intravenous morphine rescues (5 mg) and intensify laxative treatment, needing more than 15 during the day.
Following day, he was sleeping during more than 15 hours, so needing just 2 morphine rescues. Constipation was resolved and dexamethasone (adjuvant pain treatment) was added per associated soft tissue component. Also, lorazepam started every 8 hours for anxiety. As he did not vomit, oxycodone/ naloxone was reintroduced at the same dose as the beginning.
Indeed, pain was under control, so he started walking and constipation was also better. Ondansetron and oral iron were suspended (because favored constipation). Since the patient achieved a good pain management, he was discharged after first cycle of chemotherapy (Cisplatin + Etoposide) with good tolerance. Thoracic-abdominal CT after 3rd cycle showed partial response, with better symptom control, thus reducing oxycodone/naloxone to 10 mg/5 mg every 12 hours.
Afterwards, good management of symptoms at home, with water intake of 2 liters, laxatives every 12 hours and daily depositional rhythm, finally dieting at home at 11 months with a good supportive care.
Discussion
Nonetheless, when he continued vomiting and nervous, we wonder what was happening after several rotations: poor opioid tolerance? Unresolved constipation? Associated anxiety?
Initially, we have recognized neuropathic pain (although we could have associated adjuvant treatment like anticonvulsivants, antidepressants) but we should know that vomiting is not just influenced by opioid [4]. We tried to avoid oxycodone/naloxone but next day the equivalent dose of morphine was higher, so vomiting also got worse because constipation was getting worse too [5]. In addition, educating to nursing in order not to continually schedule rescues of the morphic if they are not indicated is important, because most of the times with this patient, it would be probably enough if we used benzodiacepines to relieve anxiety.
Essentially, if pain is not improving, mobility is not possible, so constipation also gets worse. If pain improves, mobility gets better and therefore constipation disappear in most of the cases [6]. Also stopping medication which favours constipation and switching again to oxycodone/naloxone is a good approach [7,8].
Apart from educating family and nursing, we should take care of the importance of hydration, antiemetics (although ondansetron favors constipation) and laxatives from the beginning.
In cases of associated anxiety, it is very important to recognize it to avoid increasing opioid doses and starting benzodiacepines/antidepressants.
Conclusion
Pain control in cancer patients is essential because of the importance on their quality of life. Controlling of tumor disease and pain behaves as a “vicious circle” because if pain is not under control, patients do not move, and constipation gets worse too. Also, opioids toxic effects are not so frequent or alarming. Suspect other causes as well: constipation due to opioids in less than 50% of cases, being also frequent because of iron, corticosteroid, ondansetron and immobilization.
Indications to rotate opioids are usually in case of neurotoxicity, intense pain that does not subside, but is not common just due to constipation. Fentanyl patch is not an ideal drug to titrate because of the latency action.
Poor pain control causes delays in starting chemotherapy that can have consequences in the prognosis of the base tumor. Elderly patients should start opioids at lower doses. Important multidisciplinary assessment.
19531
References
- Davies AN, Dickman A, Reid C (2009) The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain 13:331-338.
- Guy HH (2013) Treatment of breakthrough cancer pain: to titrate or to proportionate? Cur Med Res Opin 29: 1523-1526.
- Zepetella G, Davies A, Eijgelshoven I(2014) A network meta-analysis of the efficacy of opioid analgesics for the management of breakthrough cancer pain episodes. JPain Sympt Manag 47:772-785.
- Juan AV, Escobar Y, Casinello J, Borrega P (2012) Treatment of cancer Spain: Spanish Society of Medical Oncology (SEOM) recommendations for clinical practice. Clin Transl Oncol 14: 499-504.
- ShakeenPE (2009) Opioid equianalgesic tables: Are they all equally dangerous? J Pain Symp Manag 38: 409-417.
- Twycross RG, Hancourt JM (1991) The use of laxative at a palliative care center.Palliat Med 5:27-33.
- Meissner W, Leyendecker P, Mueller-Lissner S, Nadstawek J, Hopp M, et al. (2009) A randomised controlled trial with prolonged-release oral oxycodone and naloxone to prevent and reverse opioid-induced constipation. Eur J Pain13:56-64.
- Reimer K, Hopp M, Zenz M, Maier C, Holzer P, et al. (2009) Meetingthe challenges of opioid-induced constipation in chronic pain management:A novel approach. Pharmacology 83:10-17.