Introduction
Type 2 diabetes mellitus is a prevalent disease in the US that affects more than 15 million people. As the disease progresses over time, neuropathic pain can become a common complication. It is present in more than 50% of individuals with diabetes mellitus aged >60 years. Diabetic peripheral neuropathy (DPN) is one of the most common forms of neuropathic pain [1], and pain is the most troublesome symptom of diabetic neuropathy [2]. Of the more than 15 million people in the United States with diabetes mellitus, nearly a quarter suffers from PDN. Causes for diabetic neuropathy have not yet been determined, but risk factors include increased age, duration of diabetes, lipotoxicity and glucotoxicity, genetic susceptibility, inflammation, and oxidative stress [1,3,4].
Pain typically occurs symmetrically in the feet and ankles [5]. Patients may also have dysesthesias and paresthesias, such as crawling, itching, numbness, and tingling [6]. DPN also includes sensory and motor impairments that result in impaired gait and balance, jeopardizing safe mobility.
The main problem in treating neuropathic pain is that the standard array of non-nacrotic analgesics has little effect on neuropathic pain. The ideal in medicine is to treat the cause of a disease rather than its symptoms. Unfortunately, for patients with painful diabetic neuropahty, this is often not possible. The majority of patients require some type of medical pain management. Further research in this area is needed to investigate the effectiveness of better therapeutic protocols.
Diabetic peripheral neuropathy causes loss of distal strength and sensation with interruption of both afferent and efferent pathways. Research has shown that diabetics with peripheral neuropathy are 15 times more likely to report falling or stumbling in a one-year period [7]. The postural instability associated with diabetic peripheral neuropathy is most apparent in unipedal stance and balance – both of which are critical in gait and activities of daily living such as changing clothes and climbing stairs [8].
One retrospective study by Cavanagh et al. found that diabetic neuropathic subjects were 15 times more likely to report injury and felt significantly less safe during standing and walking than non-neuropathic subjects [9]. Another study by Richardson et al. found diabetics with EMG-confirmed peripheral neuropathy were 23 times more likely to report instability resulting in a fall or injury [10].
Emerging evidence suggests that exercise programs can be effective in improving gait and balance in general fall risk populations, as well as reducing falls and fall-related injuries [11]. Exercise interventions have been designed to reduce fall risk and maintain quality of life. These interventions come in many forms, but the most common interventions are exercise training, offered individually and in small group formats. To date no research has been done showing the effectiveness of exercise interventions for diabetic peripheral neuropathy, however; research has proven balance training to be an effective means of preventing falls in older women with osteoporosis, the elderly and chronic stroke patients. Further research is needed to gain insight into the underlying mechanisms of different type of exercises and their impact on stability in individuals with DPN. Research is also needed to determine the type or combination of types of exercise to produce a more normal and/or stable gait in these patients.
For pain management of individuals with DPN, the need for possible treatment protocols is rising. In terms of exercise protocols for improving DPN related mobility disorder, previous research utilizing resistance training has been shown to be very effective in increasing strength in older adults and clinical patients. However, there are important limitations to resistance exercise therapy in these populations, including issues of noncompliance, inability to perform these types of exercises, and an increased potential of injury in frail individuals.
As an alternative, recently whole-body vibration has been used and shown to induce many of the adaptations observed with resistance training. While whole-bodyvibration training has been shown to improve strength and balance in healthy men and women ranging between their 3rd and 8th decade of life, to our knowledge, it has yet to be applied as a treatment method for controlling pain and improving mobility disorders.
The purpose of the study was to describe a case of type II diabetic peripheral neuropathic pain with whole body vibration therapy after a failed trial of conventional drugs and interventional pain management.
Description of the Case
The patient was a 71-year old male with a 5-year history of type II diabetic peripheral neuropathic pain in his both feet. The patient was originally diagnosed with type II diabetes in 2004, and he started experiencing foot pain several months after he got diagnosed. And then he was diagnosed with diabetic peripheral neuropathy by a doctor. His pain started as an aching, partially numbness, and burning pain in his right foot, the pain was worst particularly near the medial arch of the foot. Soon after he had the pain in the right foot, he started experiencing similar pain and numbness in the left foot as well. He described that the pain in the both feet would escalate as he walks for a period of time. Besides walking, there was no particular activity that worsened the pain. Ever since he had this diabetic peripheral neuropathic pain, he has been taking Nortyptyn, however he described that the pain medication was not very effective in alleviating the pain. On physical examination (manual muscle testing), he was able to demonstrate at least 4/5- muscle strength in the both feet and ankles. When his pain in both of his feet was described by using isual analog scale (VAS), the right foot pain was 8 of 10, and the left foot pain was 6 of 10. After his pain was described, his gait and balance were tested by using a computerized gait evaluation equipment (CIR Systems, Clifton, NJ, USA) and balance testing equipment (Biodex Medical Systems, Inc. Shirley, New York).
For the balance testing, the patient became familiar with the balance machine by standing on both legs for 20 sec with the platform in its most stable position. The foot position on the platform was recorded and remained constant through each test. Once the patient acclimated to the platform, three tests were done. The patient’s arms were folded across their chest and knees will be flexed to approximately 10 – 15 degrees. All tests were performed with the patient’s eyes open. The patient was instructed to maintain a level of platform for duration of 20 seconds for each test.
The patient’s over ground walking pattern was measured on 8 m GAIT Rite mat (CIR Systems, Clifton, NJ, USA). The GAIT Rite is a walkway that measures step length, step width, stride length, step frequency, double support time, toe-in/out, and step/leg length. Age, leg length of the patient, and values from the gait parameters listed above was entered into an equation and a calculation was made to determine an individual’s stability while walking. The patient performed two passes of an 8 m path, immediately before and after each mode of walking practice, including a moving start and finish to reduce any acceleration or deceleration effect, using their usual gait aids with a seated rest at each end between passes.
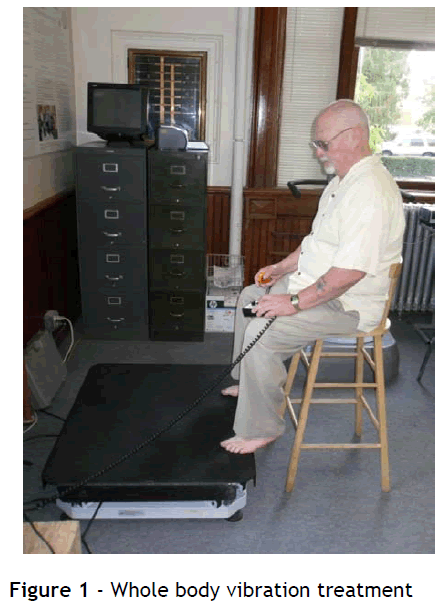
Once the baseline testing of balance and gait were completed, the whole body vibration training was initiated. The protocol for the vibration treatment consisted of 30 Hz of frequency with 5 mm of amplitude, three bouts of 2 minutes, five days a week for total 8 weeks. The patient was seated on a high chair and the foreparts of both feet were placed on the proximal edge of the vibration platform (Figure 1). The vibration treatment was applied to the bottom of both feet for 2 minutes, and the patient took a minute of rest between the bouts.
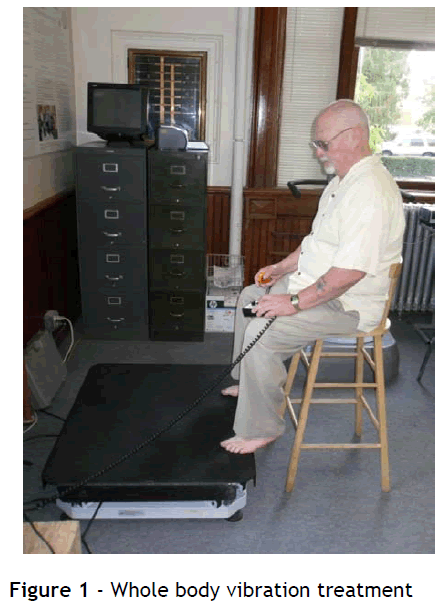
Figure 1: Whole body vibration treatment
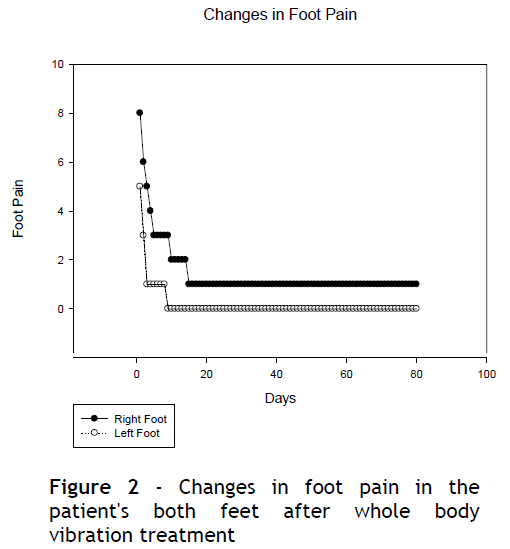
After 8 weeks of whole body vibration treatment, the patient’s pain in his both feet was significantly reduced (Figure 2). The patient rated his right foot pain as 1/10 and the left foot pain as 0/10 on a visual analog scale. It was observed that the pain in the patient's both feet was notably being reduced within two weeks of the study period. After two weeks of the treatment, the foot pain was rated as 2/10 in the right foot, and no pain in the left foot. Interesting finding during the study period was that the pain after the treatment, which the patient received in the morning, didn't come back either in the night or the morning day after.
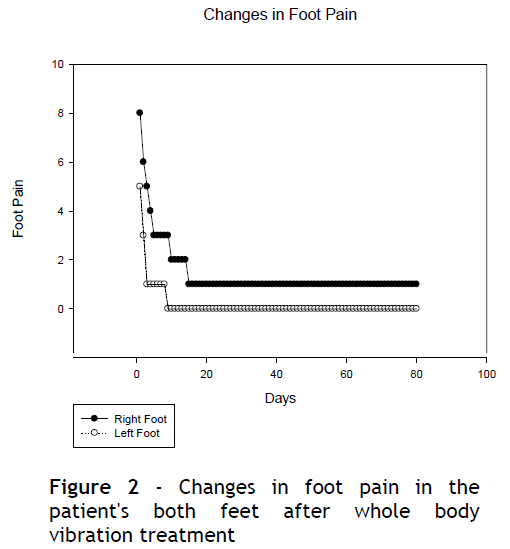
Figure 2: Changes in foot pain in the patient's both feet after whole body vibration treatment
For the gait variables, after the vibration treatment, the patient's step length, stride length, step distance, and, cadence notably increased and the patient's walking speed was notably improved (Table 1).

For the balance variables, there was no change in the limit of stability test, but there was demonstrable improvement in the postural sway testing (Figure 3).

Figure 3: Changes in balance testing scores after whole body vibration treatment
When the study was about to be completed, the patient purchased his own whole body vibration platform and continues the whole body vibration treatment to date. The patient is happy with the response and satisfied with his daily activities.
Conclusion
This study indicates that the whole body vibration treatment reduces neuropathic pain, and improves gait and balance in a patient with type II diabetic peripheral neuropathy. Although, research on this topic is in its infancy, the incorporation of whole body vibration to other therapeutic treatment option for diabetic peripheral neuropathy patients may offer promise. In this single subject study, possible placebo and learning effects cannot be completely excluded. Our report is intended to further a discussion about the possible use of whole body vibration in patients with diabetic peripheral neuropathic pain. Whole body vibration treatment warrants further investigation over the course of a longer, prospective study; in addition, long term follow up is required to help us understand if any side effects are associated with this possible therapeutic modality.
3472
References
- Schmader KE 2002 Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain 18:350?354
- Backonja M-M 1999 Gabapentin monotherapy for the symptomatic treatment of painful neuropathy: a multicenter, double-blind, placebocontrolled trial in patients with diabetes mellitus. Epilepsia 40:S57?S59
- Vinik A, Mehrabyan A 2004 Diabetic neuropathies. Med Clin North Am 88:947? 999
- Ziegler D, Sohr CGH, Nourooz-Zadeh J 2004 Oxidative stress and antioxidant defense in relation to the severity of diabetic polyneuropathy and cardiovascular autonomic neuropathy. Diabetes Care 27:2178?2183.
- Dworkin RH, Backonja M, Rowbotham MC, Allen RR, Argoff CR, Bennett GJ, Bushnell C, Farrar JT, Galer BS, Haythornthwaite Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol 60:1524? 1534
- Morello CM, Leckband SG, Stoner CP, Moorhouse DF, Sahagian GA 1999 Randomized double-blind study comparing the efficacy of gabapentin with amitriptyline on diabetic peripheral neuropathy pain. Arch Intern Med 159:1931?1937
- Turcot K, Allet L, Golay A, Hoffmeyer P, Armand S. 2009 Investigation of standing balance in diabetic patients with and without peripheral neuropathy using accelerometers. Clin Biomech 24:716-721
- Paul L, Ellis BM, Leese GP, McFrdyen AK, McMurray B 2009 The effect of a cognitive or motor task on gait parameters of diabetic patients, with and without neuropathy. Diabetic Med 26:234-239
- Cavanagh PR, Ulbrecht JS, Caputo GM 1996 Biomechanical aspects of diabetic foot disease:aetology, treatment, and prevention. Diabetic Med 13:17-22
- Richardson JK, Hurvitz EA 1995 Peripheral neuropathy: A true risk factor for falls. J of Geront 50:211-215
- Steinberg, M 2000 A sustainable programme to prevent falls and near falls in community dwelling older people: results of a randomised trial. J Epidemiol Community Health 54:227-32.