Key words
HIV, Vagina, Willingness, Microbicides, Ilorin
Introduction
Globally, HIV/AIDS infection has continued to affect millions of people and as shown in the estimates from the UNAIDS Global Reports of AIDS Epidemic, 37.2 million adults and 2.2 million children are currently living with HIV and 95% of this global estimates live in the developing world [1].
In Nigeria about 3.1percent of adults between the ages of 15-49 are living with HIV/AIDS [1]. One such risk group in Nigeria is girls who marry at a young age, causing their sexual debut to occur at an early age [2].This group, which has a mean age at first marriage of 14.6 years, is a vulnerable and largely underserved population, predominantly found in the northern part of Nigeria2. Most Nigerian undergraduates know that sexual intercourse is the most prevalent mode of HIV transmission but yet for a variety of reasons, people continue to engage in sexual behaviors which are unsafe and could put them at the risk of HIV/AIDS infection [3].
Due to the unique impact, the worldwide epidemics of Sexually Transmitted Infections especially HIV/AIDS, has on women, the demands for new preventive approaches are inevitable [4]. Also the available means of HIV prevention, ie, monogamy and fidelity, (male) condom use, and sexual abstinence are not always practical for women in resource-limited settings such as Africa [5].This urgency has led to the intense focus and growing interest in the development of vaginal microbicides research.
Topical microbicides are products that are designed to inhibit the sexual transmission of HIV and other sexually transmitted infections (STIs) [6]. Microbicides could potentially be applied vaginally, rectally, anally or on to the penis to prevent both male-to-female and female-to-male transmission; by offering a female-controlled prophylactic option, a microbicide would be an important addition to the prevention toolkit. Unfortunately, no clinical studies to date have demonstrated that these products can prevent HIV infection [7].
One of the potential advantages of vaginal microbicides is that it would not require a partner's cooperation, hence, presenting a woman-initiated prevention method. However, the effectiveness of vaginal microbicide will ultimately be influenced by women (or men’s) willingness and ability to use microbicides correctly and consistently with high risk partners [8].Acceptability research is a critical component of microbicide development process, because even a highly efficacious microbicide will not be effective if not used [9]. In developing a vaginal microbicide to protect against sexually transmitted infections (STIs), including HIV, scientists must consider not only the inherent effectiveness of any potential product but also whether women and men will use it and, if so, whether that use will be consistent [10]. For this reason, investigators are using qualitative research methods, such as in-depth interviews and focus group discussions, to determine whether women and men are likely to accept such a product [11].
Acceptability research also underscores the need to develop many types of vaginal microbicides to accommodate differing needs and conditions throughout the world. Microbicide acceptability research conducted among Zimbabwean, Mexican, and South African men, for example, found strong preferences for the development of microbicides without contraceptive properties. [12,13]
Microbicide acceptability for youth in sub-Saharan Africa may be bolstered by desperation for new methods to stop the spread of HIV, yet hindered by misgivings about experimental HIV prevention methods for youth” [14]. This study is designed to determine and identify factors that could influence the interest and acceptability of vaginal microbicides amongst youths in a tertiary health facility.
Methodology
This was a descriptive cross sectional study amongst students of University of Ilorin which is located in the capital city of Kwara found in the North-central geopolitical zone of the country. It is a modern city with recent increase in companies, social and economic infrastructure. The University of Ilorin has two campus sites namely; the mini campus and the main campus also known as the permanent site. It has eight faculties and 54 departments. Most of the students were residents in the campus initially but as the student population increased over the years, the existing halls of residence became over stretched and the university embarked on the off-campus system. Each campus has a health center and the health services provided includes both curative and preventive community health services such as Medical examination for new staff and students, Public health nursing services which includes Child Welfare and Maternity health services especially immunization of children and child care education including Family planning; Health counseling Services; Health Education and Orientation; Admission of patients into the sick bay; Minor Surgeries; Daily dressings; Laboratory services; Pharmaceutical services; School Health services at both Primary and Secondary Schools of the University.
The Multistage Sampling technique was used to select the respondents for this study. The total number of undergraduate students for 2007/2008 session is 19,523. The sample size for the study was 400.
Four faculties were selected from the eight faculties in University using simple random technique and sample required per Faculty was determined through proportionate allocation. The proportion of sampled students from each Faculty was determined from the population based on the number registered. Three departments were selected in each of the faculties using simple random sampling. In each of departments the students were selected through stratified sampling by levels (200,300,400). The total number of students in each level was obtained and the sample required was calculated based on the proportion for each level. In each level, systematic sampling technique was used to select the respondents.
The questionnaire was designed to obtain the socio-demographic data and knowledge of vaginal microbicides. After this component of the questionnaire was responded to the respondents were given written information on microbicides before their perception and willingness to accept vaginal microbicides was assessed. This was necessary because of the poor knowledge of vaginal microbicides observed during the pre-test carried at the Kwara State Polythenic. The questionnaire was self-administered. Data generated was analyzed using Epi-info version 3.2.2.
Results
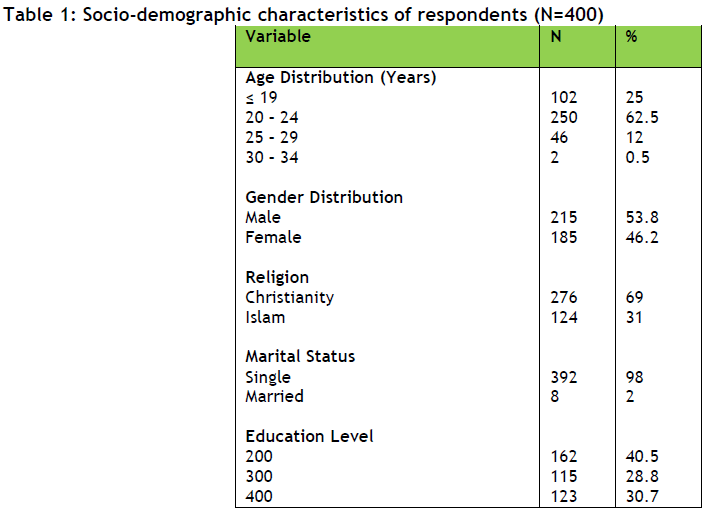
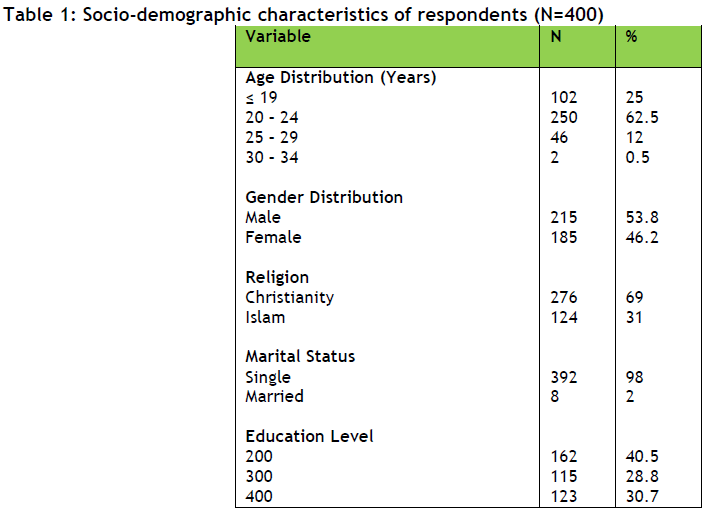
Respondents’ age ranged between 16 and 34years with a mean age of 21.6 ± 2.7years and modal age group of 20 – 24 years (Table 1). There were more males, 215 (53.8%) than females 185 (46.2%). Most of the respondents 392 (98%) were single, while 8 (2%) married.
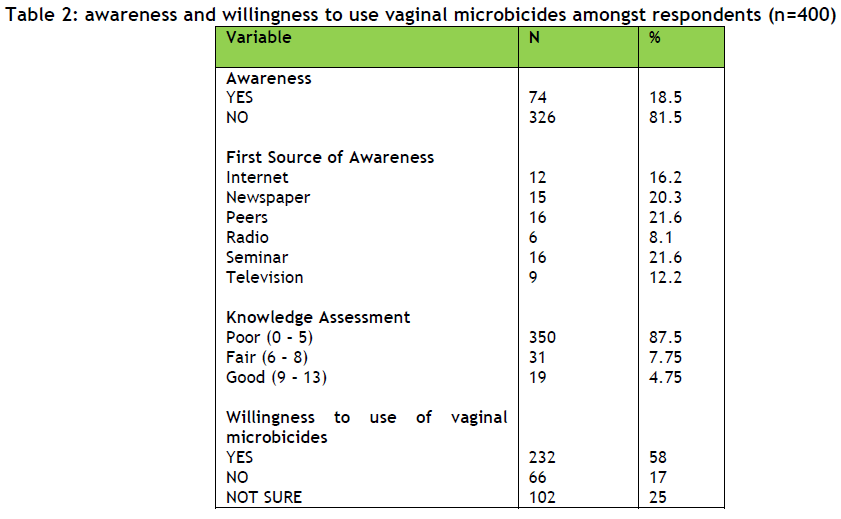
More than 80% of the respondents were unaware of vaginal microbicides which also reflected their (87.5%) poor knowledge of vaginal microbicides (Table 2) however, 12.5% had some knowledge. The most common first source of awareness indicated by most of the respondents (18.5%) who had an awareness of vaginal microbicides were through peer group or seminars, each with 21.6% respectively.
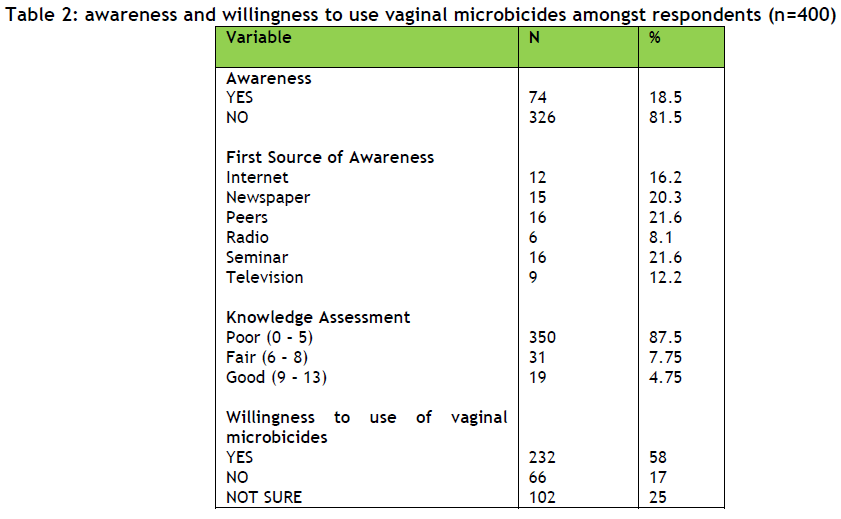
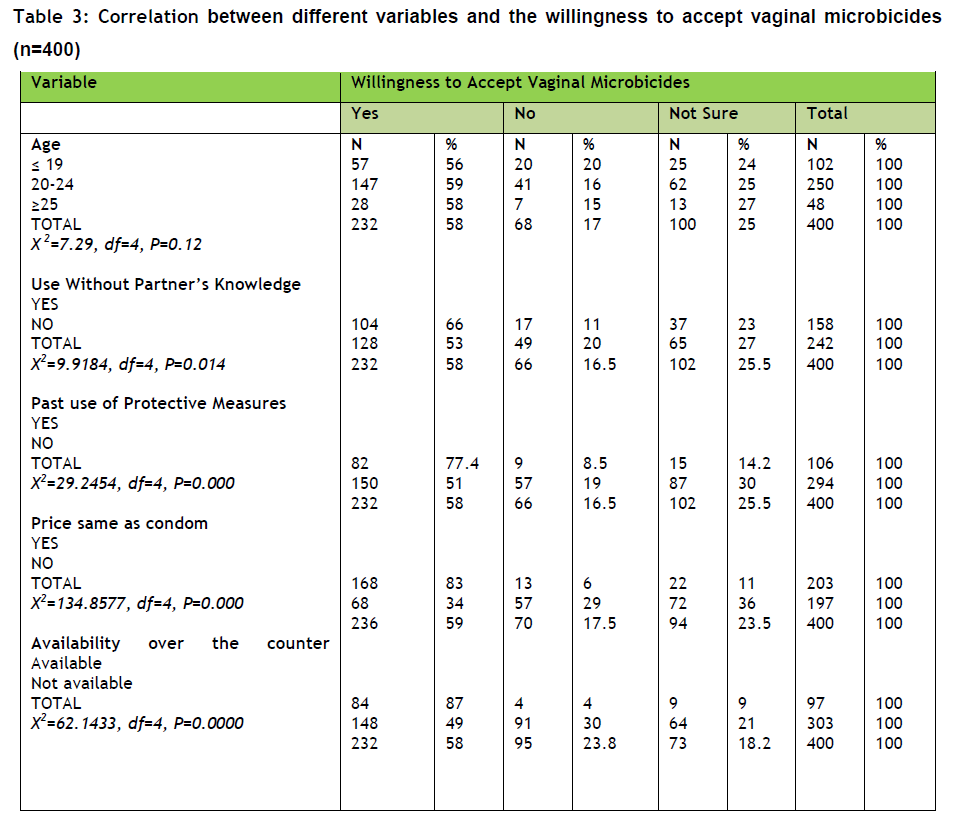
About 232, (60%) of the respondents indicated interest in the use of vaginal microbicides to protect themselves from sexually transmitted infections including HIV/AIDS of which 147 (63.4%) of these were between the ages of 20 -24 years. More than half of the respondents 232 (50.7%) were willing to accept vaginal microbicides if its price were as that of condoms’, however 197 (49.3%) of the respondents did not (Table 3).
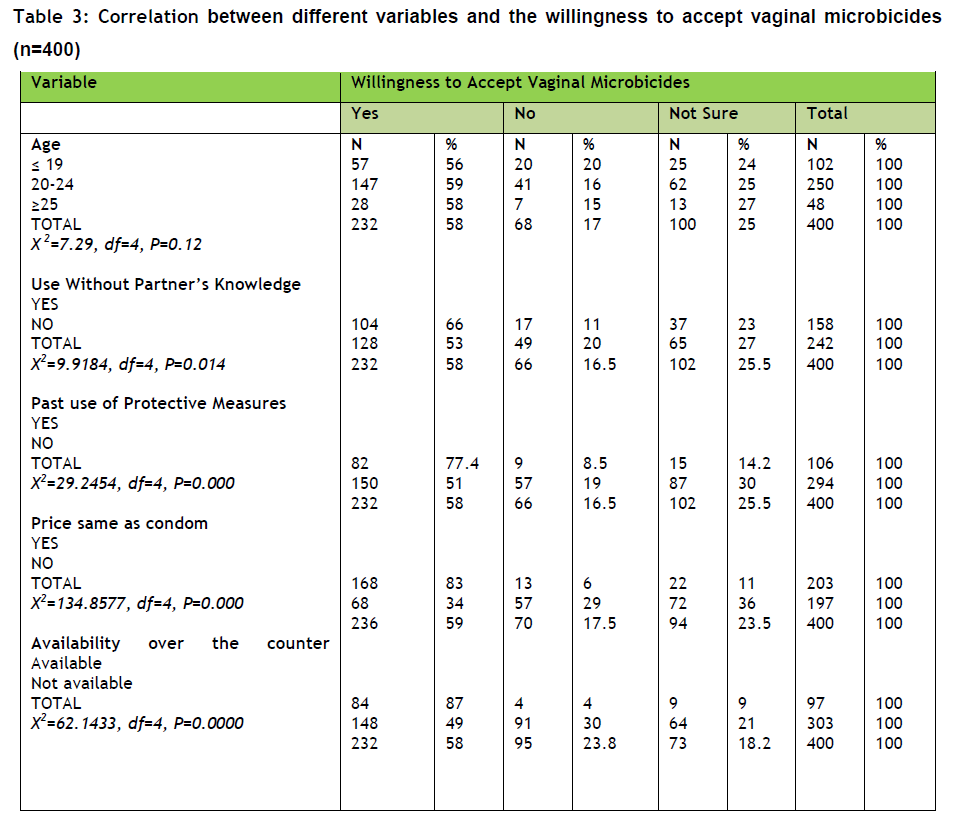
Out of 232 (58%) respondents who indicated willingness to accept the use of vaginal microbicides, 124 (66%) of the respondents felt that vaginal microbicides could be used without the knowledge of their partners while 128 (56%) felt covet use was impossible (Table 3). Most of these respondents (77.4%) had also indicated the use of a protective measure against Sexually Transmitted Infections or to prevent pregnancy during sexual intercourse in the past (Table 3).
Most of the respondents168 (83%) indicated willingness in using vaginal microbicides if the cost of vaginal microbicides were same as that of condoms’ and 84 (87%) were of the opinion that it should be accessed over the counter (Table 3).
Discussion
The age distribution (16 – 34) of the respondents in this study is consistent with the average age distribution of tertiary institutions in Nigeria. This age group has also been shown to constitute population with the highest number of persons living with HIV/AIDS [1]. Hence, this group becomes the ideal target for any HIV/AIDS prevention programme.
More than three quarters of the respondents are unaware of vaginal microbicides which is similar to the study by Smith and Adeiga et al., [13] amongst the population in Lagos where 77.5% unawareness was reported. This Low awareness is probably due to the fact that vaginal microbicides is still at the clinical trial stages with none of the clinical trials demonstrated that it could prevent HIV/AIDS [4]. Also based on the fact that there are no convincing evidences that vaginal microbicides would prevent HIV/AIDS in clinical trials, much popularity and social marketing have not been given to vaginal microbicides like the male condoms which has enjoyed popularity [15,16].
With the 74 respondents (18.5%) that are aware of vaginal microbicides, seminar and peers remain the commonest medium through which awareness was acquired. This is important in the future promotional and social marketing of reproductive commodities. It means some adolescent groups can be made as advocacy groups to mentor and influence their friends into accepting healthy sexual behavior through seminars.
General Knowledge on microbicides among the respondents is low. Eighty seven percent of the respondents have poor knowledge of vaginal microbicides which could also be adduced to the fact that vaginal microbicides is yet to be released and promoted for public consumption since it is still under clinical trials. However, the poor knowledge was in contrast to average knowledge recorded in a study conducted in South Africa among the hospital managers and Health care workers which reported average knowledge of basic knowledge of vaginal microbicides [15]. The difference could probably be adduced to the difference in the study population because the health workers are more likely to have better information, awareness of health related issues than other groups in the population.
There was a level of interest shown by the respondents (60%) in this study to microbicide usage which is similar to the study carried out in Katsina where 70% of the respondents wanted an alternative to condoms which a female can control [16]. Most of these respondents were between the ages of 20 -24 years (63.4%) age group which would be appropriate as an Advocacy group to promote the acceptance and use of vaginal microbicides especially amongst high risk groups. However, this acknowledged interest and acceptance varies with perception of the respondents on covet use (66%) and whether women would be able to protect themselves with the use of vaginal microbicides (56%).
Covet use of vaginal microbicides has been shown in this study to have a significant influence on the willingness of respondents to accept vaginal microbicides. The conception of vaginal microbicides was based on the recommendation for the development of a barrier/contraceptive method which is women-controlled and maybe used without detection by their sexual partners [8]. However, the covet use of vaginal microbicides is a controversial issue especially based on the lubricating qualities of the product. Considerations should be given to the product’s characteristics as this would impair the ability to use vaginal microbicides without partner’s knowledge which would also affect the acceptance of vaginal microbicides and willlingness to use it.
Findings from this study showed that the use of a protective measure in the past has a strong influence in determining whether vaginal microbicides would be accepted or not. It was observed that 77.4% of respondents who were willing to accept vaginal microbicides had used a protective measure in the past. This was also reported by Jacqueline et al., [17] who indicated that one of the strongest predictors of being a potential user is the respondent’s use of condoms to prevent infection with STI [17]. This shows that the perceived low-risk of sexual activity by the population is an indication of whether or not they would see the importance of protecting themselves against sexually transmitted infections. This is important especially in a society where the seeking and dissemination of information about reproductive and sexual health is misconstrued as promoting promiscuity.
It was revealed in this study that the acceptance of vaginal microbicides is significantly dependent on its cost. More than half (83%) of the respondents expressed willingness to use of vaginal microbicides if its price was similar to condoms’ which was also reported in the study carried out by Jacqueline et al., [17] where 78% expressed willingness to pay an amount equivalent to the cost of condom [17]. Although the female condom has been developed to be an innovation enabling female-controlled method, one of its problems is increased cost8 and as reported by Woodsong et al.,9 vaginal microbicides should be inexpensive to be used regularly.
Also, 87% of the respondents indicated acceptance of vaginal microbicides if made available without the need of a prescription by a health worker as also reported by Jacqueline et al., [17] where 71% of the respondents preferred that vaginal microbicides should be accessed over the counter in pharmacies or drugstore [17]. This shows that the availability of vaginal microbicides over the counter would influence the willingness to use vaginal microbicides and as such the accessibility of vaginal microbicides should be taken into consideration to aid effective use.
This study has provided insight to some factors which could influence the interest and acceptance of vaginal microbicides and the age group which would likely be more interested in the product and who would help to promote its awareness and acceptance. It is important that there should be partnership between reproductive health professionals and Patent medicine vendors, to aid accessibility and affordability of vaginal microbicides, and also to create an avenue for microbicide promotion, giving potential users an opportunity to ask questions and get accurate information. Future research efforts should address the issues on covert use which is shown in this study as an important factor influencing the interest of the population in vaginal microbicides. Finally, continuous health education programmes and seminars should be organized by institutions within and outside schools, in partnership with reproductive health professionals to address misconceptions on the use of a protective measure during sexual activity.
Conclusion/Recommendation
This study established that there is high willingness to vaginal microbicides use among the students. However its availability, cost and the possibility of covet use are influencing factors. It was recommended therefore, that these factors are to be considered in promoting its use especially amongst this high risk group.
3353
References
- Odu BK, Akanle FF. HIV/AIDS Prevention through Safer Sex Practices and Condom Use among Sexually Active Undergraduate in Nigeria. In Revitalization of African Education; In Revitalization of African Higher Education.2008. ISBN: 978-978-49117-1-9. Pg 268-277
- Musa OI, Akande TM, Salaudeen AG, Soladoye OM. Family Communication on HIV/AIDS among Secondary School Students in Northern State of Nigeria. Afri J. Infect Disease. 2008; 2(1): 46-50
- Adamson SM. Will Vaginal Microbicides Solve the HIV Problem in Africa? Craot Med J. 2006;47: 895-8.
- ENGENDERHEALTH. Paving the Path: Preparing for Microbicides Introduction Report of a Qualitative Study in South Africa.2004;28.
- UNAIDS, International Working Group on Vaginal Microbicides, Recommendations for the Development of Microbicides. AIDS 1996, 10: 1-6.
- Sharon A, Barbara F, Alana DK. December, 2008. Microbicide Acceptability Research. International Partnership for Microbicides. Available on www.ipm-microbicides.org. Accessed on the 30/03/09
- Woodsong C, Koo H. A holistic model of microbicide acceptability. Paper presented at: The Microbicides 2002; May 12-15;Antwerp, Belgium.
- Bentley M, Fullem A, Srirak N, Jogelkar N, Khumalo-Sakutukwa G, Mwatulira L. Acceptability of novel, microbicideBufferGel during a Phase I safety trial in Thailand, India, Zimbabwe, and Malawi. AIDS 2001;15(suppl 1):S30
- Elias C, Coggins C, Atisook R, Bassett M, Ettiegne-Traore V, Ghys P, et al. A Study of Women's Preferences Regarding the Formulation of Over-the-Counter Vaginal Spermicides. Critical Issues in Reproductive Health Series. New York, NY: Population Council, 1998.
- Centers for Disease Control and Prevention. Sexual, HIV Sisk and Potential Acceptability of Involving Adolescent Girls in Microbicide Research Kisunmu, Kenya. The Body. January, 2009.
- Smith .S, Adeiga .A, Agomo .C. Knowledge, Perception and Acceptability of Microbicides among Non-health Care workers in Lagos, Nigeria. Journal of Public Health. 2008;16(3): 191-194.
- Niruthisard S, Roddy RE, Chutivongse S. Use of nonoxynol-9 and reduction in rate of gonococcal and chlamydial cervical infections. The Lancet.1992; 339:1371?1375.
- Gita R, Neetha S M, James M, Joanne E M, and Varanna G. Perceptions of vaginal microbicides as an HIV prevention method among health care providers in KwaZulu-Natal, South Africa. AIDS Research and Therapy.2007;4:7
- Ukauwa CE, Akinola AA, Ukauwa LN. A comparative study of condom use and the prospect of microbicides as an alternative barrier prevention method against HIV/AIDS in Katsina State of Nigeria. Proceedings from the International Conference on AIDS; 2004 Jul 11- 16; Bankok, Thailand.
- Jacqueline E, Darrouch JF, & Jennifer JF. Women?s Interest in Vagina Microbicides. Family Planning Perspective.1999;31 (1): 16 ? 23.